Нейроэндокринные опухоли желудочно-кишечного тракта (НЭО ЖКТ) – это редкие злокачественные новообразования, которые развиваются из нейроэндокринных клеток, присутствующих во всех структурах желудочно-кишечного тракта. [1] Эти опухоли уникальны по своей природе, поскольку они способны вырабатывать гормоны. К тому же они кардинально отличаются по темпам прогрессирования – некоторые из них растут очень медленно, а для других характерен крайне агрессивный рост. [1]
За последние несколько десятилетий заболеваемость нейроэндокринными опухолями желудочно-кишечного тракта неуклонно растет во всем мире. [1] Согласно данным Программы наблюдения, эпидемиологии и конечных результатов (SEER), общая заболеваемость нейроэндокринными опухолями выросла более чем на 500% с 1970-х годов, при этом значительная доля новых случаев приходится именно на желудочно-кишечный тракт. [1]
Ввиду такого стремительного роста заболеваемости, а также появления прогрессивных методов диагностики, сейчас в фокусе внимания находятся именно инновационные виды терапии. Теперь многие пациенты желают пройти передовое лечение за рубежом, при этом Германия является одним из наиболее предпочтительных направлений для таких пациентов, ведь в этой стране прекрасно развита медицинская инфраструктура, работают клиники с международной аккредитацией и имеется экспертный опыт в области лечении сложных онкологических заболеваний.
Такие современные методы лечения, как пептид-рецепторная радионуклидная терапия (ПРРТ) с Лютецием-177 и иммунотерапия дендритными клетками, способны существенно изменить результаты лечения пациентов даже на поздних стадиях онкологического заболевания. [8-10] При раннем выявлении онкопатологии и проведении лечения в соответствии с индивидуально разработанной терапевтической схемой у многих пациентов с нейроэндокринными опухолями (НЭО) желудочно-кишечного тракта есть возможность добиться стойкой ремиссии и значительно продлить себе жизнь, что подтверждает тот факт, что у онкобольных с этим диагнозом действительно есть шанс на излечение.
Что такое нейроэндокринные опухоли желудочно-кишечного тракта?
НЭО желудочно-кишечного тракта – это гетерогенная группа редких новообразований, которые развиваются из нейроэндокринных клеток, рассеянных по всей слизистой оболочке ЖКТ. Эти специализированные клетки обладают свойствами сразу двух тканей – нервной и эндокринной, что позволяет им вырабатывать и секретировать гормоны в ответ на различные стимулы. НЭО могут развиваться в различных органах, но значительная часть этих новообразований поражает именно органы пищеварительной системы – желудочно-кишечные нейроэндокринные опухоли. [2]
Классификация НЭО ЖКТ по локализации:
- Пищевод – в этом органе такие опухоли развиваются редко, но если это все же происходит, то для них характерен агрессивный рост
- Желудок – опухоли этой локализации (нейроэндокринные опухоли желудка) классифицируют по гистологическому строению и клиническому течению
- Тонкий кишечник – тонкая кишка, включая тощую и подвздошную кишку, часто является местом локализации НЭО среднего отдела кишечника
- Аппендикс – в основном в этом органе развиваются медленно растущие опухоли небольшого размера, которые часто выявляют случайно
- Толстая кишка – на момент постановки диагноза опухоли этой локализации в большинстве случаев достигают более крупных размеров и характеризуются агрессивным ростом
- Прямая кишка – зачастую новообразования этой локализации обнаруживаются на ранней стадии благодаря рутинной скрининговой колоноскопии
- Поджелудочная железа – панкреатические нейроэндокринные опухоли (панНЭО) могут быть как функционирующими (гормонпродуцирующими), так и нефункционирующими
Развитие НЭО ЖКТ связано с несколькими факторами риска. Значительному увеличению риска возникновения таких опухолей способствуют генетические синдромы: множественная эндокринная неоплазия I типа (МЭН1), болезнь фон Гиппеля-Линдау, нейрофиброматоз I типа. К другим факторам риска относятся возраст (большинство случаев данного вида рака развивается у пациентов в возрасте 50-70 лет), курение и хронические воспалительные заболевания органов желудочно-кишечного тракта. [2]
НЭО делятся на два основных типа: функциональные и нефункциональные. Функциональные НЭО активно секретируют гормоны, например, серотонин, что приводит к таким симптомам, как приливы и диарея (карциноидный синдром). Нефункциональные НЭО в свою очередь не вырабатывают избыточного количества гормонов и часто обнаруживаются на более поздних стадиях, когда уже достигают достаточно больших размеров, из-за чего провоцируют развитие механических симптомов. [2] Эта классификация и понимание биологии опухолей играет важную роль в разработке персонализированных терапевтических схем, направленных на улучшение результатов лечения пациентов с гастроэнтеропанкреатическими нейроэндокринными опухолями.
Симптомы и диагностика НЭО ЖКТ
Гастроинтестинальные нейроэндокринные опухоли часто называют «скрытыми», поскольку они медленно растут и до достижения поздней стадии не вызывают никаких симптомов. Симптомы НЭО в значительной степени зависят от того, является ли опухоль функциональной или нефункциональной, а также от ее анатомической локализации. [1, 3]
К распространенным клиническим проявлениям данного типа рака относятся приливы, диарея и боль в животе. Реже встречаются такие симптомы, как хрипы и поражения сердечных клапанов, характерные для карциноидного синдрома, спровоцированного секрецией гормонов. У пациентов с опухолями крупных размеров могут наблюдаться обструкции, кровотечения, потеря веса. [1, 3]
В ходе диагностики при подозрении на гастроинтестинальные нейроэндокринные опухоли проводится биохимический анализ крови, эндоскопические и визуализационные исследования.
- Анализы крови и мочи: такие маркеры, как хромогранин А (CgA) и 5-гидроксииндолуксусная кислота (5-HIAA), могут указывать на наличие у пациента НЭО.
- Эндоскопия и колоноскопия: прямая визуализация и результаты биопсии имеют решающее значение, особенно при желудочных нейроэндокринных опухолях, НЭО толстой кишки, аппендикса и прямой кишки.
- Визуализационные исследования: методы поперечной визуализации, в частности КТ и МРТ, помогают оценить степень распространения онкопроцесса. Более современные методы визуализации, такие как ПЭТ/КТ с аналогами соматостатина (например, Ga-68 DOTATATE), обеспечивают высокую чувствительность при выявлении даже небольших опухолевых очагов (например, в поджелудочной железе).
- Биопсия: для выявления таких маркеров, как синаптофизин и хромогранин А, необходимо проведение иммуногистохимического исследования.
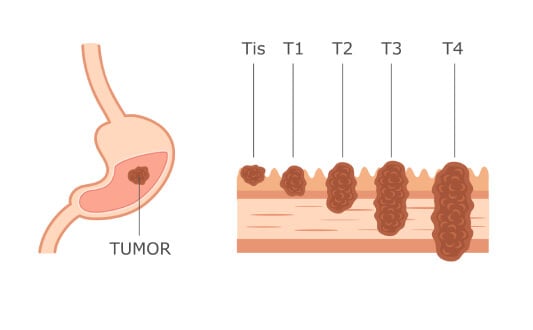
Ранняя и точная диагностика значительно расширяет возможности лечения, а также способствует улучшению терапевтических результатов для пациентов с нейроэндокринными опухолями желудка и другими НЭО желудочно-кишечного тракта. [1, 3] Вместе с тем важно отметить, что тактика лечения зачастую определяется классификацией НЭО по степени злокачественности и дифференциации.
Стандартные методы лечения в Европе
Операция – это главный метод лечения локализованных нейроэндокринных опухолей. При выявлении новообразования на ранних стадиях его полная хирургическая резекция обеспечивает наилучшие шансы на долгосрочное выживание и потенциальное излечение. Показанный пациенту вид операции определяется локализацией опухоли: например, при типе желудочных нейроэндокринных опухолей может потребоваться частичная или полная гастрэктомия, в то время как при опухолях тонкого кишечника или толстой кишки во многих случаях проводится сегментарная резекция. Хирургическая операция также помогает добиться контроля над симптомами при функциональных НЭО за счет снижения выработки гормонов и опухолевой нагрузки. [4, 5]
Химиотерапия в основном проводится пациентам с низкодифференцированными нейроэндокринными карциномами высокой степени злокачественности. Такие опухоли более агрессивны и, как правило, лучше реагируют на цитотоксические препараты. Химиотерапия менее эффективна при высокодифференцированных НЭО, но она все же выступает в качестве главного метода лечения в тех случаях, когда нужно быстро добиться контроля над заболеванием, особенно при наличии метастатических поражений. [1, 4-6]
Такие лекарства, как аналоги соматостатина (АС), широко применяются для контроля симптомов, связанных с избыточной выработкой гормонов, и замедления темпов прогрессирования опухоли. АС связываются с рецепторами соматостатина, экспрессируемыми на поверхности раковых клеток, в результате чего происходит снижение секреции гормонов и подавление роста опухоли. Такие препараты обеспечивают эффективный результат лечения у пациентов с нейроэндокринными опухолями желудка и среднего кишечника, помогая облегчить симптомы и повысить показатели беспрогрессивной выживаемости при минимальном профиле побочных эффектов. [5, 7]
Инновационные и таргетные методы лечения
Пептид-рецепторная радионуклидная терапия (ПРРТ) с Лютецием-177
Пептид-рецепторная радионуклидная терапия (ПРРТ) с Лютецием-177 (Lu-177) – это высокоточный метод лечения нейроэндокринных опухолей желудочно-кишечного тракта на поздней стадии с гиперэкспрессией рецепторов соматостатина. Принцип действия терапии основан на том, что радиоактивный изотоп Lu-177 связывается с аналогом соматостатина (например, DOTATATE), после чего он прикрепляется к раковым клеткам и обеспечивает их таргетное облучение, не затрагивая при этом окружающие здоровые ткани. [8]
Эффективность ПРРТ подтверждают результаты исследования NETTER-1, в ходе проведения которого у пациентов с поздними стадиями НЭО среднего кишечника, получавших Lu-177-DOTATATE терапию, было отмечено снижение риска прогрессирования заболевания или летального исхода на 79% по сравнению с пациентами, получавшими лишь высокие дозы октреотида LAR. [8] Кроме того, по данным исследования, в группе пациентов, получивших ПРРТ, медиана беспрогрессивной выживаемости составила около 30 месяцев по сравнению с 8,4 месяцами в контрольной группе. [8]
Подтверждением этих результатов стали и заключения немецкого многоцентрового регистрового исследования, которое продемонстрировало, что у пациентов, получавших Lu-177-DOTATATE, медиана беспрогрессивной выживаемости составила приблизительно 41 месяц, а медиана общей выживаемости – около 59 месяцев. [9]
Терапия дендритными клетками
Терапия дендритными клетками представляет собой инновационную форму иммунотерапии рака, суть которой состоит в стимуляции собственной иммунной системы пациента распознавать и уничтожать раковые клетки. Дендритные клетки – это наиболее эффективные антигенпрезентирующие клетки в организме человека, которые отвечают за запуск иммунного ответа. При проведении такого лечения осуществляется забор собственных дендритных клеток пациента, после чего их «нагружают» опухоль-специфическими антигенами и повторно вводят пациенту для «обучения» его иммунной системы атаковать раковые клетки. [10]
Основой для разработки данного вида терапии стали научные труды Ральфа Штейнмана – первооткрывателя дендритных клеток, который в 2011 году удостоился Нобелевской премии по физиологии и медицине за их открытие. Его исследования легли в основу метода вакцинации дендритными клетками для лечения рака и других заболеваний путем задействования естественных защитных механизмов организма человека. [10]
Согласно клиническим данным по лечению НЭО терапией дендритными клетками, к числу которых относятся различные солидные опухоли, в том числе рак органов желудочно-кишечного тракта, у 30-40% пациентов, прошедших вакцинацию дендритными клетками удалось добиться стабилизации заболевания. [10]
Методы интервенционной радиологии
Трансартериальная химиоэмболизация (TACE) – это малоинвазивная процедура, которая применяется для лечения метастазов нейроэндокринных опухолей желудочно-кишечного тракта в печень. Её суть состоит в доставке химиопрепарата непосредственно к опухоли печени через печеночную артерию с последующей ее эмболизацией для блокировки притока крови к новообразованию и предотвращения «утечки» лекарства из онкологического очага. Данный метод лечения работает за счет лишения опухоли питательных веществ и обеспечения максимальной концентрации химиопрепаратов непосредственно в онкологическом очаге. По результатам исследований, при метастазах НЭО в печени TACE обеспечивает объективный уровень ответа на лечение в более 90% случаев, а также в около 80% случаев процедура помогает добиться контроля над заболеванием. [11] Следует отметить, что трансартериальная химиоэмболизация выступает в качестве особо ценного терапевтического метода лечения для пациентов, которые не являются кандидатами на хирургическую резекцию.
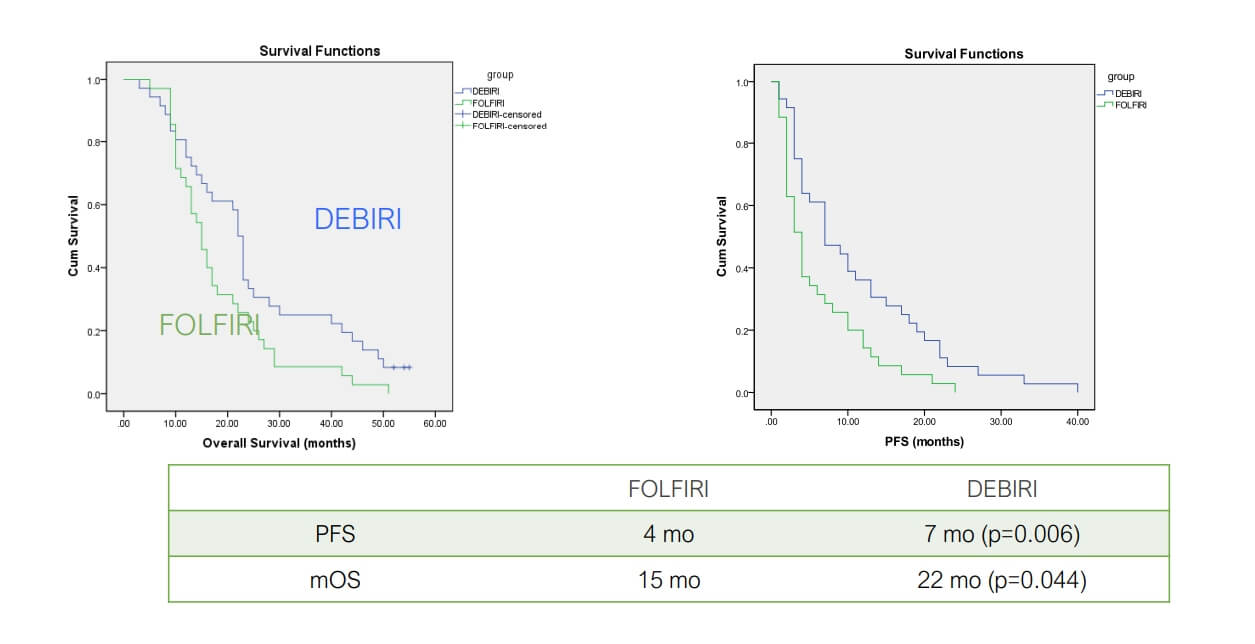
Fiorentini G et al Anticancer Res 2012;32:1387
Aliberti C et al Ancancer Res 2011;31:4581
Richardson A et al J Vasc Interv Radiol 2013;24:1209
Артериальная эмболизация (АЭ) – это еще один метод лечения рака с метастатическими поражениями печени, при котором выполняется лишь эмболизация, без таргетного введения химиопрепаратов. Целью данной процедуры является блокирование кровоснабжения опухоли, в результате чего наступает ишемия. Как правило, этот метод обеспечивает менее эффективный результат по сравнению с TACE, но АЭ подходит пациентам, которые не в состоянии перенести химиотерапевтическое лечение. Зарегистрированные показатели контроля над заболевания составляют 60-70%, при этом такая терапия менее токсична по сравнению с химиоэмболизацией. [12]
Радиочастотная абляция (РЧА) – процедура, в ходе которой для генерации тепловой энергии и разрушения с ее помощью опухолевой ткани применяется высокочастотный электрический ток. Наиболее эффективные результаты РЧА демонстрирует при опухолях небольшого размера (менее 3 см). Этот метод довольно часто применяется для лечения метастазов в печени у пациентов с НЭО. Согласно результатам исследований, частота локального контроля над опухолью при проведении РЧА составляет 80-90%, но только при условии правильного отбора пациентов. Радиочастотная абляция во многих случаях рекомендуется при невозможности проведения хирургического лечения.
Микроволновая абляция (МВА) – этот метод практически идентичный РЧА, но в этом случае для разрушения новообразования применяется микроволновая энергия, которая способна генерировать тепло более высокой температуры и создавать более крупные зоны абляции. Таким образом, МВА считается более эффективным методом для борьбы с опухолями более крупных размеров. По данным исследований, МВА обеспечивает сопоставимые или даже немного лучшие показатели локального контроля над опухолью по сравнению с РЧА, при этом показатели успешности лечения при метастазах НЭО в печени составляют более 90%.
Криоабляция – это терапевтическая процедура, предполагающая замораживание опухолевой ткани, в результате чего в раковых клетках формируются кристаллы льда и происходит их разрушение. Этот метод отличается особой эффективностью при опухолях с локализацией вблизи жизненно важных анатомических структур, поскольку в таких случаях термоабляция сопряжена с риском их сопутствующего повреждения. В настоящее время доступно не так много научных данных по результатам лечения НЭО желудочно-кишечного тракта этим методом, но общие показатели в онкологии свидетельствуют о том, что при проведении криоабляции метастазов печени частота локального контроля над заболеванием составляет около 70-80%.
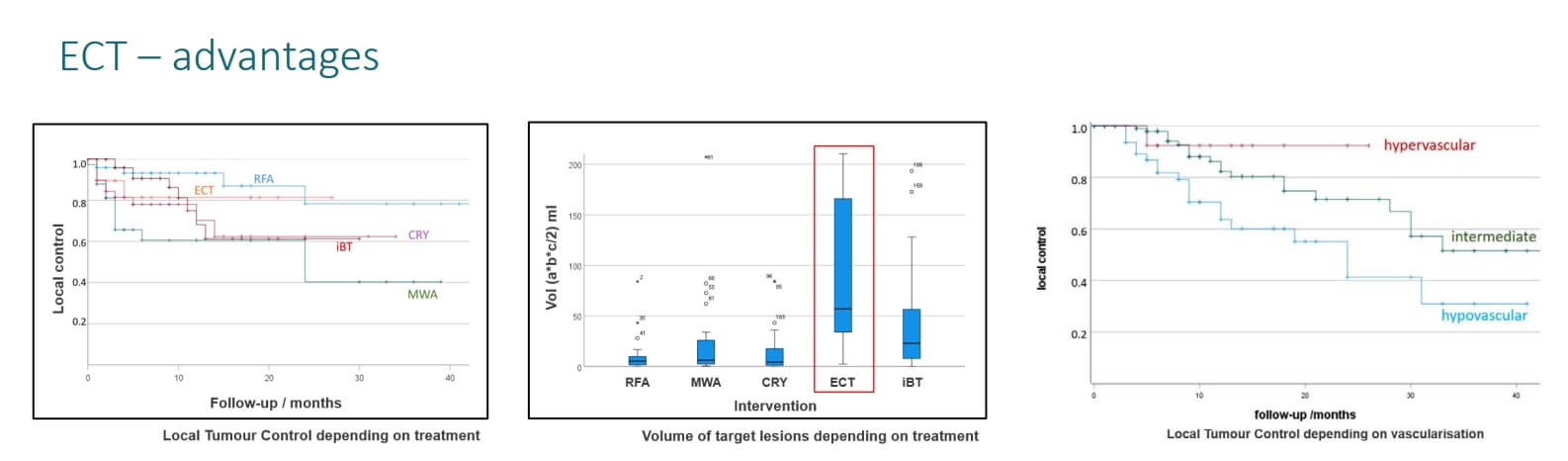
Электрохимиотерапия (ЭХТ) – инновационная процедура, предполагающая сочетание таргетной химиотерапии с локальным воздействием на опухоль электрическими импульсами, благодаря которым повышается проницаемость клеточной мембраны и обеспечивается лучшее проникновение лекарственных препаратов в раковые клетки. В настоящее время применение ЭХТ для лечения нейроэндокринных опухолей желудочно-кишечного тракта все еще находится на стадии изучения, но предварительные данные свидетельствуют о достижении контроля над заболеванием в 70-85% случаев.
| Вид терапии | Показатели 2-летней выживаемости | Показатели ответа на лечение | Продолжительность курса лечения | Побочные эффекты |
|---|---|---|---|---|
| Стандартные методы лечения | ~25% на поздних стадиях рака | Менее 10% | Несколько циклов | Тяжелые побочные эффекты (тошнота, повышенная утомляемость, выпадение волос, иммуносупрессия, раздражение кожи) |
| Инновационные методы лечения | ~60% на поздних стадиях рака | 45-65% | До 4 сеансов | Незначительные побочные эффекты (дискомфорт в месте проведения лечебной манипуляции) |
*Данные Booking Health
Стоимость лечения НЭО ЖКТ в разных странах мира
| Метод лечения | Германия* | Великобритания | США |
|---|---|---|---|
| Стандартные методы лечения | €80 000 - €150 000 за полный курс | €90 000 - €165 000 за полный курс | €100 000 - €180 000 за полный курс |
| Инновационные методы лечения | €25 000 - €60 000 за полный курс | €70 000 - €120 000 за полный курс | €100 000 - €150 000 за полный курс |
*Цены могут варьироваться в зависимости от конкретного курса лечения и особенностей диагностированной у пациента опухоли
Возможности лечения за границей
Для многих пациентов с диагнозом «нейроэндокринная опухоль желудочно-кишечного тракта» лечение за рубежом открывает перспективы к получению более прогрессивной и персонализированной медицинской помощи по сравнению с тем уровнем медицинского обслуживания, которое предлагается на родине. В ряде стран, особенно в некоторых государствах Европы, в протоколы лечения не всегда входят инновационные методики, поскольку здесь действуют более длительные процессы одобрения новых видов терапии или же вовсе ограничен доступ к передовым технологиям.
Напротив, ведущие европейские центры, особенно медучреждения в Германии, предоставляют доступ к инновационным методам лечения, включая ПРРТ с Лютецием-177, передовые интервенционные вмешательства под визуальным контролем и персонализированную иммунотерапию, например, терапию дендритными клетками. Немецкие клиники славятся своей интеграцией прогрессивных диагностических методов, в том числе ПЭТ/КТ с Ga-68 DOTATATE, и междисциплинарными командами врачей, которые разрабатывают для каждого пациента индивидуальные схемы лечения.
Помимо предоставления пациентам самых прогрессивных методов лечения, клиники в Германии также завоевали безупречную репутацию благодаря своим высоким стандартами ухода за больными, коротким срокам ожидания записи на прием к врачу и прозрачной структуре формирования стоимости терапии, что способствует улучшению общих результатов лечения для иностранных пациентов. Для многих выбор в пользу лечения в Германии означает не только доступ к лучшим терапевтическим методикам, но также возможность улучшить прогноз и качество жизни, а во многих случаях и полностью восстановить свое здоровье.
Лечение в Германии
Как уже упоминалось, Германия зарекомендовала себя как мировой лидер в лечении НЭО ЖКТ. В этой стране пациенты могут получить медицинскую помощь в профильных онкологических центрах, специализирующихся на лечении нейроэндокринных опухолей (НЭО). Терапевтический процесс координируется междисциплинарными командами врачей, состоящими из онкологов, хирургов, радиологов, специалистов по нуклеарной медицине, патологоанатомов.
Возможности лечения в Германии выходят за рамки традиционных подходов, благодаря чему врачам удается существенно улучшать показатели беспрогрессивной выживаемости и качество жизни пациентов с нейроэндокринными опухолями желудка и НЭО желудочно-кишечного тракта. К тому же в Германии обеспечивается более быстрый доступ к новым методам лечения и терапии в рамках клинических исследований. Также многие немецкие онкологические центры принимают активное участие в научно-исследовательских проектах и разработке инноваций, благодаря чему пациенты относительно быстро получают доступ к новейшим разработкам в области лечения нейроэндокринных опухолей. Все это способствует тому, что Германия по-прежнему удерживает лидирующие позиции на международной медицинской арене и продолжает привлекать пациентов со всего мира с этими редкими и сложными опухолями, желающих получить наилучший результат лечения.
Как начать лечение за границей и во сколько оно обойдется?
Стоимость лечения нейроэндокринных опухолей желудочно-кишечного тракта может значительно различаться в зависимости от страны, в которой оно будет проводится, и выбранного вида терапии. В Германии стоимость стандартных методов лечения, например, хирургического вмешательства и химиотерапии, варьируется в пределах €80 000 - €150 000, в то время как лечение инновационными методами, например, ПРРТ с Лютецием-177 и терапией дендритными клетками, обойдется в €25 000 - €60 000 за полный курс. По сравнению с другими странами, например, США или Великобританией, в Германии пациентам предлагается передовое медицинское обслуживание по более конкурентоспособным ценам.
С Booking Health начать лечение за границей довольно просто. Компания поможет с решением таких вопросов:
- Оценка медицинских заключений: ведущие специалисты проводят первичную оценку медицинских заключений пациента с целью разработки предварительной схемы лечения.
- Сбор документов: специалисты компании помогают собрать необходимый пакет медицинских документов и перевести их на немецкий для передачи в выбранную пациентом для лечения клинику.
- Подбор клиники: сотрудники компании позаботятся об индивидуальном подборе лучших клиник в Германии с учетом особенностей вашего клинического случая.
- Помощь в оформлении визы и организации поездки в Германию: при сотрудничестве с Booking Health пациент получает полную поддержку в организации поездки в Германию, бронировании отеля или апартаментов для проживания на период лечения и подаче документов на визу с гарантией эффективность процесса.
Благодаря услугам Booking Health у пациентов с такими сложными заболеваниями, как нейроэндокринные опухоли, есть возможность получить доступ к высококлассному медицинскому обслуживанию международного стандарта и улучшить результаты лечения, получая при этом рекомендации на каждом этапе процесса.
Подбор наилучшего варианта лечения в вашей индивидуальной клинической ситуации с Booking Health
Выбор оптимальной тактики лечения нейроэндокринной опухоли – это весьма сложная задача. Многие пациенты с нейроэндокринными опухолями желудочно-кишечного тракта сталкиваются с рядом трудностей из-за посещения многочисленных консультаций, ограничений стандартных протоколов лечения и сложной для понимания информации, которую они получают от врачей. В такой ситуации онкобольные часто соглашаются на лечение традиционными методами. При этом тот факт, что такая терапия обеспечивает не особо эффективные результаты и вызывает серьезные побочные эффекты отходит на второй план. К счастью, современная медицина предлагает передовые персонализированные методы лечения, которые действительно способны помочь пациенту восстановить здоровье. Первый шаг на пути к получению доступа к этим терапевтическим методикам – осознанный выбор пациента.
В Германии предлагаются самые передовые методы лечения нейроэндокринных опухолей желудочно-кишечного тракта. Здесь имеется уникальный экспертный опыт в области проведения таких инновационных процедур, как ПРРТ с Лютецием-177, TACE, терапия дендритными клетками. Специалисты немецких клиник проводят точную диагностику и инновационное лечение, обеспечивая эффективную помощь пациентам с гастроэнтеропанкреатическими нейроэндокринными опухолями с различных уголков мира.
Booking Health занимается организацией персонализированного лечения рака за рубежом уже более 12 лет. Как надежный партнер, мы оказываем всестороннюю поддержку на каждом этапе вашего лечения. Мы предлагаем:
- Оценку и анализ медицинских заключений пациента
- Составление индивидуальной медицинской программы
- Подбор наиболее подходящей клиники в Германии
- Подготовку медицинской документации и ее направление в выбранную пациентом для лечения клинику
- Консультации с ведущими врачами в Германии на этапе подготовки к поездке на лечение
- Полная поддержка во время пребывания в больнице
- Помощь в оформлении визы, бронировании авиабилетов и трансфера, а также номера в отеле или апартаментов на период лечения
- Услуги персонального координатора и переводчика
- Прозрачные цены на лечение без скрытых платежей
В Booking Health мы убеждены, что здоровье – главная ценность в жизни каждого человека, доверять заботу о которой стоит лишь лучшим специалистам. Мы поможем вам получить доступ к услугам лучших экспертов и новейшим методам лечения нейроэндокринных опухолей желудочно-кишечного тракта.
Свяжитесь с врачом-консультантом компании уже сегодня, и он поможет вам узнать больше о том, как персонализированное лечение в Германии способно помочь вам добиться лучших результатов и более высокого качества жизни.
Современная онкология: опыт пациентов Booking Health
Частые вопросы наших пациентов о нейроэндокринных опухолях желудочно-кишечного тракта
Отправить запрос на лечениеНейроэндокринные опухоли желудочно-кишечного тракта – это редкие злокачественные новообразования, которые развиваются из нейроэндокринных клеток, присутствующих в слизистой оболочке пищеварительной системы. Эти опухоли способны вырабатывать гормоны. Как правило, они локализуются в желудке, тонком кишечнике, толстой кишке и прямой кишке.
Возникновение НЭО желудочно-кишечного тракта часто связано с генетическими факторами, например, множественной эндокринной неоплазией 1-го типа (МЭН1), хроническими воспалительными процессами или спорадическими мутациями. Тем не менее, точная причина развития этого типа рака пока неизвестна, поэтому продолжаются исследования для ее определения.
Симптомы различаются в зависимости от локализации и типа опухоли. В основном заболевание проявляется дискомфортом в желудке, язвами двенадцатиперстной кишки, ректальными кровотечениями, диареей, приливами, болью в животе. Во многих случаях НЭО не вызывают никаких симптомов до достижения онкопроцессом поздних стадий.
В ходе обследования при подозрении на нейроэндокринную опухоль желудочно-кишечного тракта проводится анализов крови, визуализационные исследования, например, ПЭТ/КТ, и эндоскопическая биопсия. Нейроэндокринные опухоли желудка часто обнаруживаются во время планового эндоскопического исследования.
Какой метод лечения нейроэндокринных опухолей желудочно-кишечного тракта считается наиболее эффективным?
Оптимальный метод лечения нейроэндокринных опухолей желудочно-кишечного тракта определяется в зависимости от размера опухоли, ее локализации и степени распространения. Возможные варианты лечения включают хирургическое вмешательство, ПРРТ с Лютецием-177 и таргетные лечебные процедуры.
Да, в Германии доступны инновационные методы лечения НЭО. В ведущих клиниках для лечения нейроэндокринных опухолей желудочно-кишечного тракта предлагаются передовые терапевтические методики, например, ПРРТ, TACE, иммунотерапия дендритными клетками.
ПРРТ с Лютецием-177 – это таргетный метод лечения нейроэндокринных опухолей, предполагающий таргетное облучение раковых клеток, экспрессирующих рецепторы соматостатина, без вреда для здоровых тканей.
Да, при НЭО желудочно-кишечного тракта применяется вакцинация дендритными клетками и терапия ингибиторами контрольных точек иммунного ответа в рамках клинических исследований.
Показатели выживаемости при нейроэндокринных опухолях желудочно-кишечного тракта варьируются в зависимости от степени злокачественности опухоли и ее стадии. При локализованном новообразовании 5-летняя выживаемость превышает 80%, но на поздних стадиях заболевания она существенно снижается.
Стоимость лечения НЭО в Германии составляет €25 000 - €60 000 при применении инновационных видов терапии и €80 000 - €150 000 за полный курс лечения по стандартному протоколу в зависимости от сложности конкретного клинического случая.
К числу таких клиник относятся Университетские клиники Гейдельберга, Мюнхена и Берлина, которые славятся своим экспертным опытом в области лечения нейроэндокринных опухолей желудочно-кишечного тракта.
Чтобы пройти лечение за рубежом, следует обратиться в Booking Health. Сотрудники компании ознакомятся с медицинскими заключениями и подготовят необходимую документацию, а также помогут с выбором клиники и организацией поездки, окажут полную поддержку на протяжении всего терапевтического процесса.
Во многих случаях при локализованных НЭО желудочно-кишечного тракта операция является методом лечения первой линии, но при наличии у пациента метастазов или при неоперабельных опухолях чаще всего предпочтение отдают таким альтернативным методам, как ПРРТ или эмболизация.
Функциональные НЭО желудочно-кишечного тракта вырабатывают гормоны, что провоцирует развитие таких клинических симптомов, как приливы или диарея, в то время как нефункциональные НЭО не вызывают никаких симптомов и часто никак не проявляются до достижения поздних стадий.
Да, Booking Health специализируется на организации лечения для пациентов с нейроэндокринными опухолями в Германии с учетом их индивидуальных потребностей, обеспечивая им доступ к услугам ведущих специалистов и инновационным видам терапии.
Выбирайте лечение за рубежом и Вы, несомненно, получите отличный результат!
Авторы:
Статья составлена под редакцией экспертов в области медицины, врачей-специалистов доктора Надежды Иванисовой и доктора Вадима Жилюка. Для лечения состояний, о которых идет речь в статье, необходимо обратиться к врачу; информация в статье не предназначена для самолечения!
С редакционной политикой, которая отражает наше стремление к точности и прозрачности, можно ознакомиться здесь. Перейдите по ссылке, чтобы ознакомиться с нашими правилами.
Источники:
[1] JAMA Oncology. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. https://jamanetwork.com/journals/jamaoncology/fullarticle/2621997
[2] ScienceDirect. Nothing But NET: A Review of Neuroendocrine Tumors and Carcinomas. https://www.sciencedirect.com/science/article/pii/S1476558617303470
[3] The Lancet Oncology. Gastroenteropancreatic neuroendocrine tumours. https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(07)70410-2/abstract
[4] National Comprehensive Cancer Network. Neuroendocrine and Adrenal Tumors. https://www.nccn.org/professionals/physician_gls/pdf/neuroendocrine.pdf
[5] Journal of the National Comprehensive Cancer Network: JNCCN. Neuroendocrine and Adrenal Tumors, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. https://jnccn.org/view/journals/jnccn/19/7/article-p839.xml
[6] Journal of Neuroendocrinology. European Neuroendocrine Tumor Society 2023 guidance paper for functioning pancreatic neuroendocrine tumour syndromes. https://onlinelibrary.wiley.com/doi/10.1111/jne.13318
[7] Journal of Clinical Oncology. Placebo-Controlled, Double-Blind, Prospective, Randomized Study on the Effect of Octreotide LAR in the Control of Tumor Growth in Patients With Metastatic Neuroendocrine Midgut Tumors: A Report From the PROMID Study Group. https://ascopubs.org/doi/10.1200/JCO.2009.22.8510
[8] New England Journal of Medicine. Phase 3 Trial of 177 Lu-Dotatate for Midgut Neuroendocrine Tumors. https://www.nejm.org/doi/10.1056/NEJMoa1607427
[9] European Journal of Cancer. Effectiveness and side-effects of peptide receptor radionuclide therapy for neuroendocrine neoplasms in Germany: A multi-institutional registry study with prospective follow-up. https://www.ejcancer.com/article/S0959-8049(16)00047-2/abstract
[10] Nature Reviews Cancer. Cancer immunotherapy via dendritic cells. https://www.nature.com/articles/nrc3258
[11] Springer Nature Link. Transarterial chemoembolization for liver metastases of a pancreatic neuroendocrine neoplasm: a single-center experience. https://link.springer.com/article/10.1007/s00595-023-02714-9
[12] American Cancer Society. Hepatic arterial embolization and chemoembolization for the treatment of patients with metastatic neuroendocrine tumors. https://acsjournals.onlinelibrary.wiley.com/doi/10.1002/cncr.21389
Читайте:
Лечение рака на поздних стадиях: новейшие методы и технологии в борьбе с метастазами
Комплексная иммунотерапия рака в ведущих клиниках Германии
Комплексная иммунотерапия рака дендритными клетками в Германии
Меню статьи:
- Что такое нейроэндокринные опухоли желудочно-кишечного тракта?
- Симптомы и диагностика НЭО ЖКТ
- Стандартные методы лечения в Европе
- Инновационные и таргетные методы лечения
- Сравнительная таблица с данными по методам лечения НЭО ЖКТ за рубежом
- Возможности лечения за границей
- Как начать лечение за границей и во сколько оно обойдется?
- Подбор наилучшего варианта лечения в вашей индивидуальной клинической ситуации с Booking Health
- Частые вопросы наших пациентов о нейроэндокринных опухолях желудочно-кишечного тракта
Не знаете, с чего начать?
Свяжитесь с Booking Health