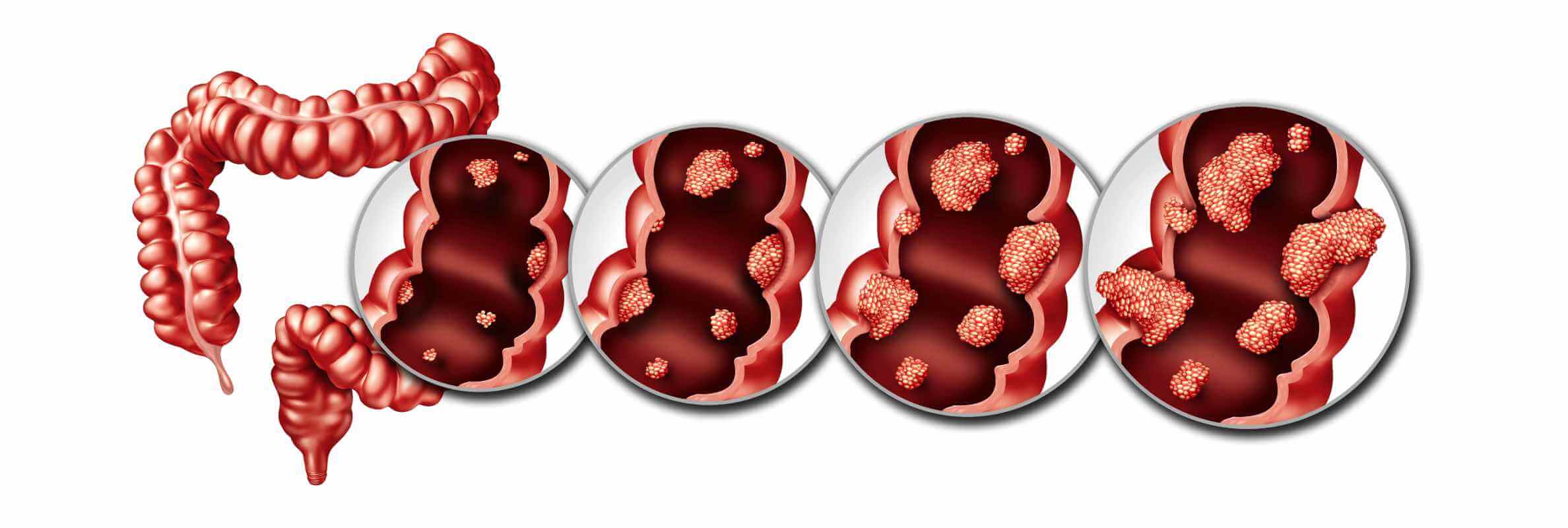
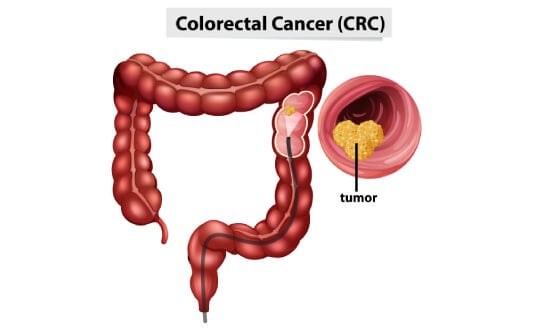
При 4 стадии колоректального рака происходит метастазирование – распространение раковых клеток за пределы толстой и прямой кишки. Эти клетки могут поражать отдаленные органы, в частности печень, легкие или брюшину. Колоректальный рак 4 стадии считается наиболее тяжелой и агрессивной формой заболевания. По данным Всемирной организации здравоохранения, колоректальный рак занимает третье место по распространенности среди онкологических заболеваний в мире: ежегодно регистрируется более 1,9 миллиона новых случаев заболевания и более 930 000 смертей от этой онкопатологии [1]. Примерно у 20% пациентов этот вид рака диагностируется на 4 стадии, когда уже присутствуют метастазы в отдаленных органах [2]. Пятилетняя выживаемость при колоректальном раке 4 стадии составляет порядка 13% [3], но этот показатель может варьироваться. Прогноз выживаемости зависит от многих факторов, включая общее состояние пациента, степень распространения метастазов и проводимый курс лечения.
Зачастую пациенты и их близкие воспринимают диагноз «поздняя стадия рака» как приговор, но на самом деле не все так плохо, ведь в последние годы появилось множество инновационных медицинских разработок для борьбы с колоректальным раком 4 стадии. Традиционные методики, например, химиотерапия, дополняются инновационными таргетными видами терапии, которые в некоторых случаях способны обеспечить даже более эффективный результат, чем лечение по стандартному протоколу. Безусловно, 4 стадия колоректального рака – это серьезный диагноз, но современная медицина предлагает множество вариантов лечения этого онкологического заболевания. Благодаря внедрению в клиническую практику новаторских терапевтических схем, которые адаптируются к конкретному клиническому случаю пациента, многие онкобольные с метастатическим колоректальным раком теперь живут дольше и ведут более полноценную жизнь.
Традиционные методы лечения
Химиотерапия уже долгое время считается основным методом лечения колоректального рака 4 стадии [4]. Во многих случаях она используется в качестве лечения первой линии для уменьшения размеров опухоли, замедления прогрессирования заболевания и облегчения симптомов. При метастатическом раке химиотерапия также играет важную роль в качестве паллиативного метода лечения – в таком случае она направлена не на излечение рака, а на улучшение качества жизни пациента и повышения показателей выживаемости. Как правило, стандартные схемы лечения химиотерапией подразумевают применение этого метода в комбинации с таргетной терапией с целью повышения общей эффективности лечения.
Принцип действия таргетной терапии основан на нарушении механизмов работы специфических белков или генетических мутаций, способствующих росту опухоли. Оптимальный для пациента вид таргетной терапии подбирается на основании индивидуального молекулярно-генетического профиля диагностированной у него опухоли. Таргетные препараты направлены на повышение точности и эффективности химиотерапии, что способствует более успешному лечению поздних стадий колоректального рака.
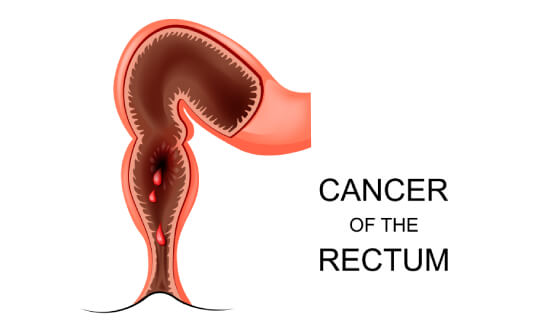
Паллиативная лучевая терапия назначается пациентам, которые испытывают дискомфорт из-за размера опухоли или ее локализации. Как правило, в процессе лечения рака толстой кишки облучение не проводится, но оно обеспечивает эффективный результат при опухолях прямой кишки или метастатических поражениях, провоцирующих внутренние кровотечения, болевой синдром или непроходимость кишечника.
Роль хирургического вмешательства в лечении колоректального рака 4 стадии весьма ограничена. Тем не менее, в некоторых случаях операция все же имеет крайне важное значение: порой при колоректальном раке метастатические поражения присутствуют лишь в одном органе, например, печени или легких, и в такой клинической ситуации проведение хирургической резекции первичной опухоли и метастатических очагов потенциально способно обеспечить пациенту длительную ремиссию. Однако такое лечение могут получить лишь отдельные пациенты с благоприятным диагнозом и минимальным риском развития рецидива.
Инновации в лечении поздних стадий рака
До недавнего времени лечение колоректального рака 4 стадии было преимущественно направлено на замедление прогрессирования заболевания и купирование симптомов, но благодаря возможностям современной медицины сейчас пациентам предлагается более персонализированная терапия. В настоящее время онкологи отдают предпочтение мультимодальным схемам лечения, позволяющим комплексно воздействовать на злокачественную опухоль.
Терапия дендритными клетками
Одним из наиболее инновационных методов в области современной иммунотерапии рака толстой кишки является терапия дендритными клетками при раке кишечника. При этом методе лечения для выявления и уничтожения раковых клеток задействуется собственная иммунная система пациента. Терапия дендритными клетками является одним из немногих методов лечения, который отличается эффективностью даже при борьбе с метастатическим колоректальным раком 4 стадии.
Дендритные клетки – это специализированные иммунные клетки, которые распознают чужеродные антигены и «обучают» другие иммунные клетки атаковать их. Лечение дендритными клетками состоит из таких этапов:
- Выделение дендритных клеток из образца крови пациента
- «Знакомство» дендритных клеток с опухоль-специфическими антигенами в лабораторных условиях, зачастую аденокарциномы (наиболее распространенного типа колоректального рака)
- После «обучения» распознаванию опухоль-специфических антигенов дендритные клетки повторно вводятся пациенту с целью запуска таргетного противоракового иммунного ответа
Научную основу этой терапии заложил канадский иммунолог Ральф Штейнман, которому в 2011 году посмертно была присуждена Нобелевская премия по физиологии и медицине за открытие дендритных клеток и их центральной роли в адаптивном иммунитете [5].
Как правило, терапия дендритными клетками проводится в комплексе с другими методами лечения, например, терапией ингибиторами контрольных точек иммунного ответа или химиотерапией с целью повышения ее эффективности. Данный терапевтический подход расценивается в качестве особо важного варианта лечения резистентных или рецидивирующих форм колоректального рака при отсутствии эффекта от стандартного лечения. Согласно результатам клинических исследований, терапия дендритными клетками способствует повышению показателей беспрогрессивной выживаемости и замедлению прогрессирования заболевания, а также в некоторых случаях способна обеспечить достижение частичной или полной ремиссии.
Гипертермическая интраперитонеальная химиотерапия (HIPEC)
При лечении колоректального рака 4 стадии с метастазами в брюшину – распространением раковых клеток на серозную оболочку, выстилающую внутренние стенки брюшной полости, – стандартная химиотерапия часто оказывается малоэффективной. В таких случаях отдельным пациентам предлагается HIPEC – новый вид регионарного химиотерапевтического лечения, при котором подогретый раствор лекарственных препаратов вводится непосредственно в брюшную полость.
HIPEC проводится в комбинации с циторедуктивной операцией (ЦРО) [6]. Лечение методом HIPEC предполагает:
- Хирургическое удаление видимых опухолей в брюшной полости
- Промывание брюшной полости подогретым раствором химиопрепаратов сразу же после операции
- Улучшение поглощения химиопрепаратов раковыми клетками за счет их нагрева, что способствует повышению эффективности лекарственных средств, – HIPEC помогает уничтожить оставшиеся микроскопические раковые клетки, минимизируя при этом повреждение здоровых тканей
Этот метод обеспечивает эффективный результат пациентам с карциноматозом брюшины на фоне опухолей прямой или сигмовидной кишки, поскольку возможности системной химиотерапии при метастатическом поражении этих отделов кишечника весьма ограничены. Исследования демонстрируют, что у отдельных пациентов проведение ЦРО в сочетании с HIPEC способно увеличить 5-летнюю выживаемость до 51%.
Представляем вашему вниманию эксклюзивное интервью с профессором Михаэлем Липпом – главврачом отделения абдоминальной и колоректальной хирургии Клиники Асклепиос Бармбек Гамбург. В нем специалист рассказывает о том, что в настоящее время именно проведение циторедуктивной операции в комбинации с HIPEC обеспечивает наиболее эффективный результат при лечении карциноматоза брюшины, особенно у пациентов с колоректальным раком.
Профессор Михаэль Липп о преимуществах HIPEC и важной роли метода в современном лечении колоректального рака
Внутрибрюшная аэрозольная химиотерапия под давлением (PIPAC)
Альтернативой гипертермической интраперитонеальной химиотерапии является PIPAC. Данная лечебная процедура представляет собой оптимальный вариант лечения для пациентов с колоректальным раком 4 стадии и обширными метастазами в брюшину, которым противопоказано проведение открытой операции. Внутрибрюшная аэрозольная химиотерапия под давлением – это малоинвазивный метод лечения, предполагающий распыление химиотерапевтических препаратов в виде аэрозоля непосредственно в брюшной полости во время проведения лапароскопического вмешательства.
В отличие от традиционных методов доставки химиопрепаратов, в ходе PIPAC они распыляются в виде мелкодисперсного тумана, что обеспечивает их более равномерное и глубокое проникновение в опухолевые ткани. Процедуру можно проводить повторно каждые 6-8 недель. Как правило, она хорошо переносится пациентами. Лечение методом PIPAC рекомендуют на поздних или терминальных стадиях заболевания, когда в приоритете не излечение от онкопатологии, а обеспечение пациенту паллиативной помощи.
Согласно клиническим данным, медиана выживаемости при проведении внутрибрюшной аэрозольной химиотерапии под давлением варьируется от 8 до 37,8 месяцев – в зависимости от стадии заболевания и ранее проводимых лечебных мероприятий. Важно, что при прохождении лечения методом PIPAC у пациентов наблюдается улучшение качества жизни, а также по сравнению с системной химиотерапией процедура вызывает меньшее количество побочных эффектов.
Методы интервенционной радиологии
Проведение лечения с применением методов интервенционной радиологии (ИР) предполагает использование прогрессивных технологий визуализации для обеспечения контроля при выполнении малоинвазивных процедур, в ходе которых врачи таргетно воздействуют на опухоль. Методы интервенционной радиологии расцениваются в качестве важного варианта лечения для пациентов с метастазами в печени, а также для онкобольных, которые из-за возраста или сопутствующих заболеваний не в состоянии перенести системное лечение.
Радиочастотная абляция (РЧА) и микроволновая абляция (МВА) – это методы, которые широко применяются для лечения метастазов в печени размером менее 3 см. При проведении обеих процедур для прицельного уничтожения раковых клеток без повреждения здоровых тканей печени применяется тепловая энергия. Согласно результатам исследований, проведение РЧА и МВА у отдельных пациентов обеспечивает локальный контроль над опухолью в 80-90% случаев и 5-летнюю выживаемость более чем в 50% случаев. Эти процедуры:
- Являются малоинвазивными, в основном проводятся чрескожным доступом под контролем КТ или УЗИ
- Могут выполняться повторно, благодаря чему есть возможность проводить лечение новых метастатических очагов по мере их появления
- Во многих случаях применяются в качестве составляющей мультимодальной схемы лечения в сочетании с системной терапией или хирургическим вмешательством для обеспечения пациенту лучших результатов
Криоабляция предполагает воздействие на раковые клетки экстремально низкими температурами с целью их заморозки и последующего разрушения. Метод имеет особую ценность при лечении опухолей с локализацией вблизи жизненно важных анатомических структур, таких как кровеносные сосуды, нервы или желчные протоки. В отличие от процедур термоабляции данный вид терапии способствует снижению риска сопутствующего повреждения чувствительных анатомических участков. Основные преимущества криоабляции:
- Минимальные болевые ощущения после проведения лечебной процедуры и быстрые сроки восстановления
- Визуализация «ледяного шара» в режиме реального времени, за счет чего обеспечивается таргетное воздействие на опухоль
- Эффективный вариант лечения для пациентов с противопоказаниями к проведению хирургического вмешательства или РЧА
Во многих случаях врачи отдают предпочтение проведению криоаблации при лечении опухолей в труднодоступных анатомических участках или при ограниченных возможностях терапии в конкретном клиническом случае пациента.
При проведении электрохимиотерапии (ЭХТ) таргетное введение низкой дозы химиопрепаратов сочетается с одномоментным воздействием на онкологический очаг короткими электрическими импульсами. Благодаря этому улучшается поглощение лекарственных средств раковыми клетками. За счет воздействия на опухоль электрическими импульсами в клеточных мембранах временно формируются поры, что обеспечивает более эффективное проникновение химиопрепаратов в раковые клетки. ЭХТ отличается высокой эффективностью при лечении метастатических поражений печени на фоне колоректального рака – в около 85,7% случаев наблюдается объективный ответ на лечение. Медиана беспрогрессивной выживаемости при проведении электрохимиотерапии составляет около 9 месяцев. Преимущества ЭХТ:
- Обладает хорошей переносимостью и минимальной системной токсичностью
- Эффективна при рецидивирующих и резистентных к терапии опухолях
- Зачастую проводится под визуальным контролем для обеспечения высокой точности таргетного введения лекарственных препаратов
Электрохимиотерпия считается оптимальным вариантом лечения нерезектабельных вторичных новообразований в печени при колоректальном раке, в том числе опухолей с труднодоступной локализацией или локализацией в участках печени, на которых ранее проводились те или иные лечебные манипуляции.
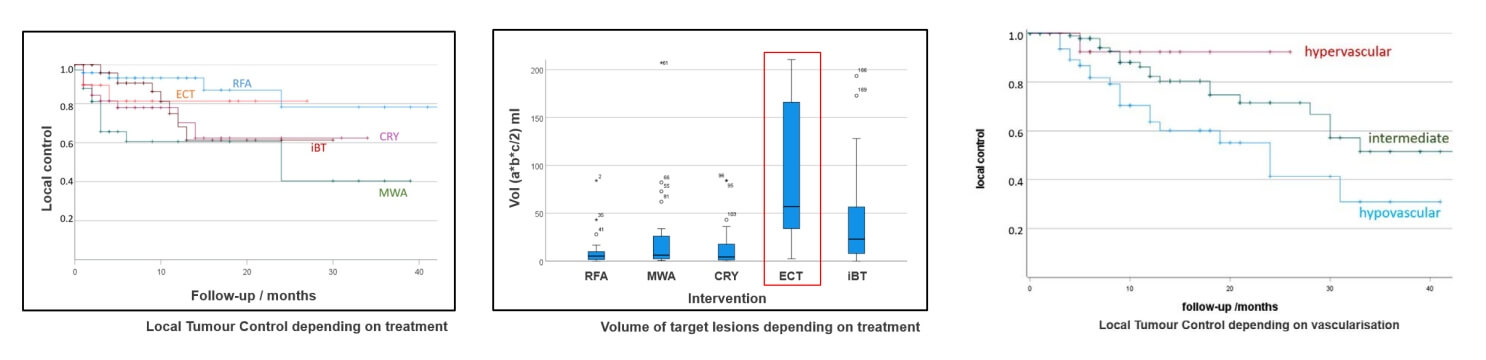
Артериальная эмболизация (АЭ) – это метод лечения, суть которого состоит в блокировке кровеносных сосудов, обеспечивающих приток крови к опухоли. В результате проведения АЭ злокачественное новообразование лишается кислорода и питательных веществ. Процедура отличается особой эффективностью при лечении гиперваскулярных метастазов в печени. В некоторых случаях она применяется в сочетании с регионарной химиотерапией (химиоэмболизацией). Преимущества артериальной эмболизации:
- Малоинвазивная процедура, которую при необходимости можно проводить повторно
- Выполняется интервенционными радиологами под контролем ангиографии
- Служит альтернативным вариантом лечения при невозможности проведения хирургического вмешательства или выполняется в качестве паллиативной терапии для уменьшения опухолевой нагрузки
АЭ помогает улучшить контроль над опухолью и облегчить болевой синдром. В некоторых случаях данный метод лечения также способствует улучшению показателей выживаемости пациентов с метастатическими поражениями печени на фоне колоректального рака.
Стентирование зачастую рекомендуется пациентам с колоректальным раком 4 стадии, когда возникает необходимость в немедленной декомпрессии кишечника. У пациентов с поздними стадиями рака кишечника на фоне роста опухоли развивается непроходимость кишечника, которая существенно ухудшает качество жизни онкобольного. Для восстановления проходимости кишечника и нормальной функции органа под контролем флюороскопии или эндоскопии устанавливается металлический стент.
Процедура стентирования:
- Обеспечивает кратковременное облегчение болевого синдрома перед проведением куративного (излечивающего) хирургического вмешательства в тех случаях, когда это возможно
- Выступает в качестве паллиативного варианта лечения для пациентов с неоперабельным колоректальным раком
- Практически исключает необходимость проведения экстренного хирургического вмешательства и сокращает сроки госпитализации
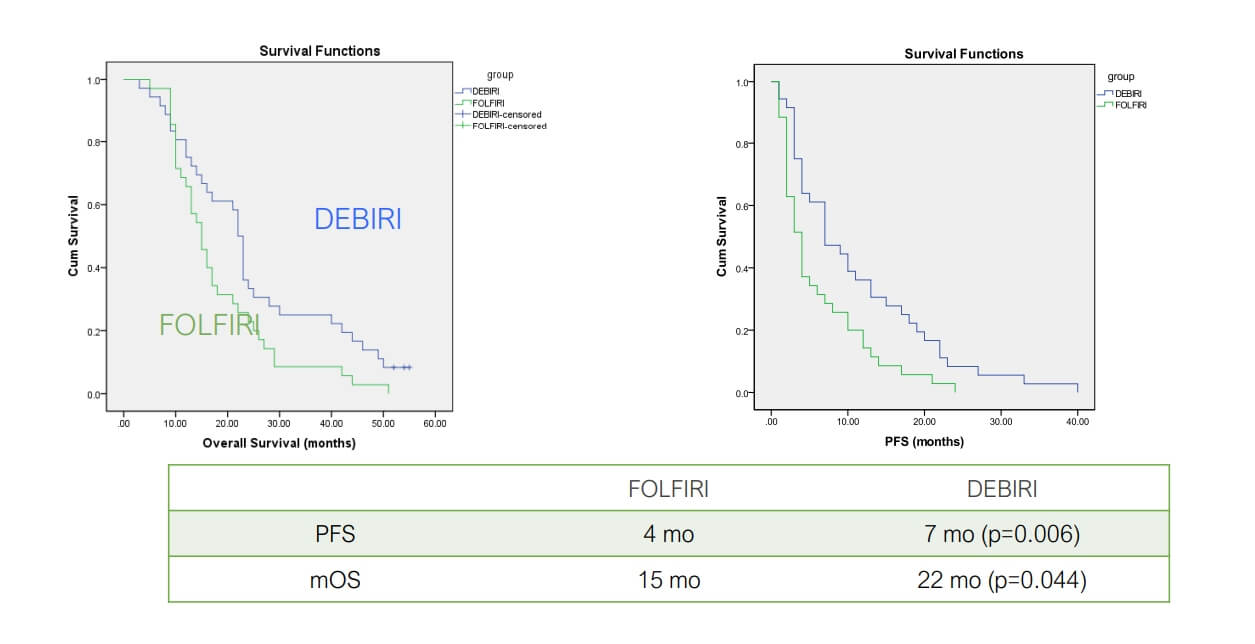
Трансартериальная химиоэмболизация (TACE) – это эффективный малоинвазивный метод лечения, таргетно воздействующий непосредственно на опухоли печени [7]. Этапы проведения TACE:
- В печеночную артерию, кровоснабжающую печень, вводится катетер
- Непосредственно к опухолевому очагу доставляются химиопрепараты
- На завершающем этапе процедуры в просвет кровоснабжающей новообразование артерии вводятся эмболизирующие микрочастицы, блокирующие приток крови к опухоли
Преимущество TACE с применением эмболизирующих микросфер с лекарственным покрытием заключается в прицельном воздействии высококонцентрированной дозой химиопрепаратов на опухоль с одномоментным лишением ее кислорода и питательных веществ.
Aliberti C et al Ancancer Res 2011;31:4581
Richardson A et al J Vasc Interv Radiol 2013;24:1209
Следовательно, при проведении TACE снижается системная токсичность лечения и улучшается ответ опухоли на терапию. Согласно результатам клинических исследований, TACE позволяет достичь контроля над заболеванием в 54,3% случаев, а медиана общей выживаемости после такого лечения составляет 47,4 месяца.
К тому же трансартериальную химиоэмболизацию можно проводить повторно. Процедура хорошо переносится пациентами. Для обеспечения онкобольному наилучших результатов лечения TACE во многих случаях проводится в сочетании с системной химиотерапией или иммунотерапией. У многих пациентов с неоперабельными формами колоректального рака 4 стадии процедура TACE способствует увеличению продолжительности жизни и улучшению ее качества.
Гипертермия
Гипертермия представляет собой инновационный терапевтический метод, который применяется в рамках мультимодального лечения колоректального рака 4 стадии и других злокачественных новообразований органов желудочно-кишечного тракта на поздних стадиях. Суть данной лечебной процедуры состоит в следующем: температура опухолевых тканей преднамеренно повышается до 40-43°C (104-109.4°F), за счет чего улучшается эффективность химиотерапии и лучевой терапии, а также одномоментно обеспечивается прямое повреждение раковых клеток.
Гипертермия отличается высокой эффективностью при:
- Раке кишечника 4 стадии и раке прямой кишки 4 стадии с обширной локальной инвазией или метастазами
- Лечении рака тонкого кишечника с труднодоступной локализацией опухоли для ее хирургической резекции
- Лечении рака двенадцатиперстной кишки в сочетании с системной терапией для достижения лучшего локального контроля над новообразованием
Гипертермия способствует усилению притока крови к опухолям, что в свою очередь обеспечивает эффективную доставку высококонцентрированной дозы химиопрепаратов к раковым клеткам. Данная процедура также повышает чувствительность раковых клеток к химиотерапии и лучевой терапии, за счет чего улучшается ответ на стандартные методы лечения. Кроме того, гипертермия напрямую повреждает раковые клетки, нарушая их функции и вызывая апоптоз (запрограммированную гибель клеток).
Одним из основных преимуществ гипертермии является ее неинвазивность или минимальная инвазивность в зависимости от применяемого метода – локальная гипотермия или гипертермия всего тела. Данный метод может стать важным дополнением к терапевтической схеме пациентов, получающих лечение рака кишечника 4 стадии, ведь гипертермия не только повышает эффективность традиционных видов терапии, но также способствует улучшению показателей беспрогрессивной выживаемости и общих результатов лечения.
| Вид терапии | Показатели 2-летней выживаемости | Показатели ответа на лечение | Продолжительность курса лечения | Побочные эффекты |
|---|---|---|---|---|
| Стандартные методы лечения | ~25% на поздних стадиях рака | Менее 10% | Несколько циклов | Тяжелые побочные эффекты (тошнота, повышенная утомляемость, выпадение волос, иммуносупрессия, раздражение кожи) |
| Инновационные методы лечения | ~60% на поздних стадиях рака | 45-65% | До 4 сеансов | Незначительные побочные эффекты (дискомфорт в месте проведения лечебной манипуляции) |
*Данные Booking Health
Стоимость медицинских процедур для лечения колоректального рака в разных странах мира
| Метод лечения | Германия* | Великобритания | США |
|---|---|---|---|
| Стандартные методы лечения | €80 000 - €150 000 за полный курс | €90 000 - €165 000 за полный курс | €100 000 - €180 000 за полный курс |
| Инновационные методы лечения | €25 000 - €60 000 за полный курс | €70 000 - €120 000 за полный курс | €100 000 - €150 000 за полный курс |
*Цены могут варьироваться в зависимости от назначенного пациенту курса лечения и особенностей опухоли
История пациентки об успешном лечении рака методом TACE
У пациентки Сарасибалы Премачандран из Великобритании диагностировали колоректальный рак 4 стадии с метастазами в печени. Лечение традиционными методами в ее родной стране оказалось безуспешным, поэтому ее семья решила начать поиски вариантов лечения за рубежом и обратилась за помощью в Booking Health.
Сарасибала отправилась в Германию, где прошла процедуру TACE в Университетской клинике им. Гёте во Франкфурте. Лечение лично проводил профессор Томас Фогль – всемирно известный эксперт в области интервенционной онкологии. Терапия была подобрана с учетом состояния пациентки. Системная химиотерапия на родине Сарасибалы не дала желаемого результата, в то время как проведение процедуры TACE в Германии обеспечило локальное уничтожение метастазов в печени.
Дочь пациентки, Суганди, отметила не только высококачественную медицинскую помощь, но и исключительную поддержку со стороны Booking Health: «Благодаря специалистам Booking Health у нас не было трудностей в процессе организации лечения в Германии. Сотрудники компании подробно рассказывали о каждом предстоящем этапе процесса, обеспечили перевод сложной медицинской информации, а также следили за тем, чтобы мы чувствовали себя в безопасности и у нас не было никаких сложностей в ходе лечения в чужой стране».
Благодаря сочетанию профессиональной медицинской помощи и качественных координационных услуг в настоящее время качество жизни Сарасибалы существенно улучшилось.
Современная онкология: опыт пациентов Booking Health
Инновационные методы лечения рака – новая надежда для пациентов
Диагноз колоректальный рак 4 стадии повергает пациента в шок. После таких слов, как «метастатический» и «терминальный», пациенты часто теряют всякую надежду на излечение. Даже врачи, действующие из лучших побуждений, могут утверждать, что в этом случае пациенту вряд ли что-то поможет. На самом деле у онкобольного всегда есть шанс получить эффективное лечение.
Современная медицина развивается стремительными темпами. Сейчас доступны новые терапевтические методики, которые меняют перспективы лечения поздних стадий рака. Они открываю реальные возможности в тех клинических случаях, которые ранее считались неизлечимыми. Традиционные методы лечения, например, химиотерапия, по-прежнему играют важную роль в борьбе с онкологическими заболеваниями, но при многих опухолях развивается резистентность к химиопрепаратам, а также побочные эффекты существенно ухудшают качество жизни пациента. Именно в таких ситуациях индивидуально составленная схема лечения с применением инновационных методик может кардинально изменить исход терапии.
Такие передовые методы лечение, как иммунотерапия дендритными клетками, трансартериальная химиоэмболизация (TACE) и таргетная молекулярная терапия, разработаны для взаимодействия с организмом пациента. Эти виды терапии лучше переносится онкобольными и зачастую обеспечивают более эффективный результат даже при метастатическом раке.
В Booking Health мы верим, что каждый заслуживает на качественное и эффективное лечение международного стандарта. Мы предоставляем пациентам доступ к лучшим специалистам, инновационным терапевтическим протоколам и всесторонней поддержке в ходе лечения.
Поездка на лечение за границу с Booking Health
Поиск оптимальных методов лечения колоректального рака 4 стадии представляет собой довольно сложную задачу, особенно когда вы сталкиваетесь с противоречивыми мнениями, сложными терапевтическими протоколами и эмоциональным истощением. Специалисты Booking Health помогают пациентам принимать обоснованные решения: при сотрудничестве с компанией вам будет предоставлен выбор из нескольких программ лечения, составленных с учетом особенностей вашего клинического случая в кооперации с ведущими онкологами Европы.
Booking Health имеет более 12 лет опыта в области координации сложных медицинских программ по лечению рака в зарубежных клиниках. Сотрудники компании гарантируют каждому пациенту доступ к передовым методам лечения, высокоточной диагностике и обслуживанию высококлассными врачами. Мы предлагаем:
- Комплексную оценку медицинских заключений пациента
- Составление индивидуальной программы лечения
- Подбор подходящего медицинского учреждения и специалистов
- Перевод и подготовку медицинской документации
- Обеспечение прямой коммуникации с ведущими специалистами перед началом лечения за границей
- Экспертные консультации во время пребывания в больнице
- Координационные услуги после завершения курса лечения и помощь в организации последующего наблюдения
- Помощь в оформлении визы, бронировании авиабилетов и номера в отеле или апартаментов на период лечения
- Услуги переводчика и персонального координатора, который будет с вами на связи 24/7
- Прозрачные цены на лечение без скрытых платежей
Мы позаботимся о каждом аспекте вашей поездки на лечение за рубеж, предоставляя вам возможность полностью сосредоточиться на своем выздоровлении вместо решения логистических вопросов. Здоровье – главная ценность в жизни каждого человека, доверять заботу о которой стоит лишь лучшим специалистам с богатым опытом и проверенной репутацией.
Booking Health – это ваш надежный партнер, который оказывает всестороннюю помощь на пути к восстановлению здоровья и улучшению качества жизни. Свяжитесь с врачом-консультантом компании, чтобы узнать больше о возможностях персонализированного лечения метастатического колоректального рака у ведущих экспертов с использованием инновационных методов.
Частые вопросы о колоректальном раке 4 стадии
Отправить запрос на лечениеКолоректальный рак 4 стадии (метастатический колоректальный рак) – это наиболее тяжелая стадия заболевания, при которой происходит распространение (метастазирование) онкопроцесса на отдаленные органы, в частности печень, легкие или брюшину.
К распространенным симптомам колоректального рака 4 стадии относятся боль в животе, ректальное кровотечение, потеря веса, повышенная утомляемость, изменения в работе кишечника и симптомы, возникающие на фоне распространения метастазов (например, желтуха или одышка).
В ходе диагностики проводится колоноскопия с биопсией, а также КТ или МРТ, ПЭТ/КТ и анализы крови, в том числе на онкомаркеры, например, РЭА (раково-эмбриональный антиген).
Продолжительность жизни значительно варьируется в зависимости от локализации опухоли, степени метастазирования и ответа на лечение. Благодаря инновационным методам лечения многие пациенты теперь могут прожить не один год после постановки диагноза.
Пятилетняя выживаемость при колоректальном раке 4 стадии составляет около 13%, но при проведении интенсивного курса лечения, составленного для пациента в индивидуальном порядке, этот показатель может быть выше.
Полное излечение на этой стадии рака встречается редко, особенно при наличии у пациента обширных метастатических поражений. Тем не менее, у некоторых пациентов удается достичь длительной ремиссии, особенно при небольшом количестве метастазов и хорошем ответе на лечение.
При колоректальном раке 4 стадии проводится химиотерапия, таргетная терапия, иммунотерапия, HIPEC, TACE, PIPAC, терапия дендритными клетками и интервенционные вмешательства под визуальным контролем. Наиболее эффективные результаты лечения обеспечиваются при выборе в пользу мультимодальной схемы терапии.
Химиотерапия остается одним из основных методов лечения колоректального рака 4 стадии. Она проводится в комплексе с таргетной терапией или регионарными видами терапии. Химиотерапия помогает уменьшить размер опухоли, облегчить симптомы и продлить онкобольному жизнь.
Да. Иммунотерапия, включая лечение ингибиторами контрольных точек иммунного ответа и терапию дендритными клетками, используется при лечении опухолей с мутациями MSI-H/dMMR или же в качестве составляющей мультимодальных схем лечения.
Прогноз зависит от нескольких ключевых факторов: общего состояния пациента, количества и локализации метастазов, а также доступности инновационных методов лечения. Многим пациентам удается добиться контроля над онкологическим заболеванием и повысить продолжительность жизни.
Побочные эффекты различаются в зависимости от предоставляемого метода лечения. Они могут включать повышенную утомляемость, тошноту, невропатию, выпадение волос, иммуносупрессию. Инновационные методы лечения во многих случаях вызывают меньше побочных эффектов, при этом они не такие тяжелые, как при стандартных видах терапии.
Да, такие истории существуют. Многие пациенты, такие как Сарасибала Премачандран, решились на лечение с применением инновационных методик, например, TACE, что позволило им восстановить качество жизни. Такие пациенты являются живым доказательство того, что даже при колоректальным раком 4 стадии есть возможность добиться выздоровления.
Выбирайте лечение за рубежом и Вы, несомненно, получите отличный результат!
Авторы:
Статья составлена под редакцией экспертов в области медицины, врачей-специалистов доктора Надежды Иванисовой и доктора Богдана Михальнюка. Для лечения состояний, о которых идет речь в статье, необходимо обратиться к врачу; информация в статье не предназначена для самолечения!
С редакционной политикой, которая отражает наше стремление к точности и прозрачности, можно ознакомиться здесь. Перейдите по ссылке, чтобы ознакомиться с нашими правилами.
Источники:
[1] WHO. Colorectal cancer. https://www.who.int/news-room/fact-sheets/detail/colorectal-cancer
[2] PubMed Central. Stage IV Colorectal Cancer at Initial Presentation versus Progression during and after Treatment, Differences in Management: Management Differences for Initial Presentation versus Progression of Disease after Initial Treatment. https://pmc.ncbi.nlm.nih.gov/articles/PMC10843884/
[3] Medical News Today. How long will a person with stage 4 colon cancer live? https://www.medicalnewstoday.com/articles/325230
[4] American Cancer Society. Chemotherapy for Colorectal Cancer. https://www.cancer.org/cancer/types/colon-rectal-cancer/treating/chemotherapy.html
[5] PubMed. The 2011 Nobel Prize in physiology or medicine. https://pubmed.ncbi.nlm.nih.gov/22053831/
[6] PubMed. Hyperthermic intraperitoneal chemotherapy in colorectal cancer. https://pubmed.ncbi.nlm.nih.gov/38722737/
[7] World Journal of Surgical Oncology. Efficacy of transarterial chemoembolization with drug-eluting beads combined with systemic chemotherapy and targeted therapy in colorectal cancer liver metastasis. https://wjso.biomedcentral.com/articles/10.1186/s12957-023-03253-w
Читайте:
Колоректальный рак: комплексное руководство по методам лечения
Меню статьи:
- Традиционные методы лечения
- Инновации в лечении поздних стадий рака
- Сравнительная таблица с данными по методам лечения колоректального рака за рубежом
- История пациентки об успешном лечении рака методом TACE
- Инновационные методы лечения рака – новая надежда для пациентов
- Поездка на лечение за границу с Booking Health
- Частые вопросы о колоректальном раке 4 стадии
Не знаете, с чего начать?
Свяжитесь с Booking Health