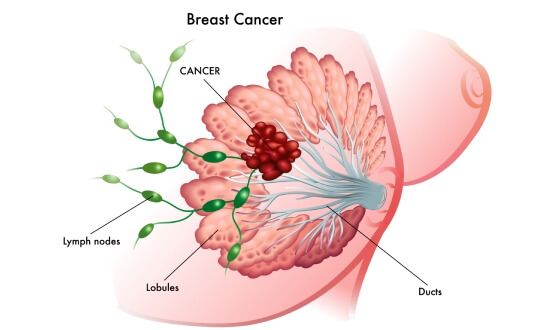
Рак молочной железы является наиболее распространенным злокачественным заболеванием среди женщин в Европе. Это гетерогенное заболевание, патогенез которого в большинстве случаев остается неизвестным. На сегодняшний день медицинскому сообществу удалось добиться значительного прогресса в ранней диагностике и лечении рака молочной железы, что привело к улучшению показателей выживаемости пациенток. Различные молекулярные подтипы рака молочной железы характеризуются различной органотропностью метастазирования [1]. Несмотря на применение современных схем мультимодальной терапии, у 30% пациенток развивается рецидив заболевания, при этом у 64% онкобольных отмечается появление отдаленных метастазов, а у 12% – изолированных метастазов [2].
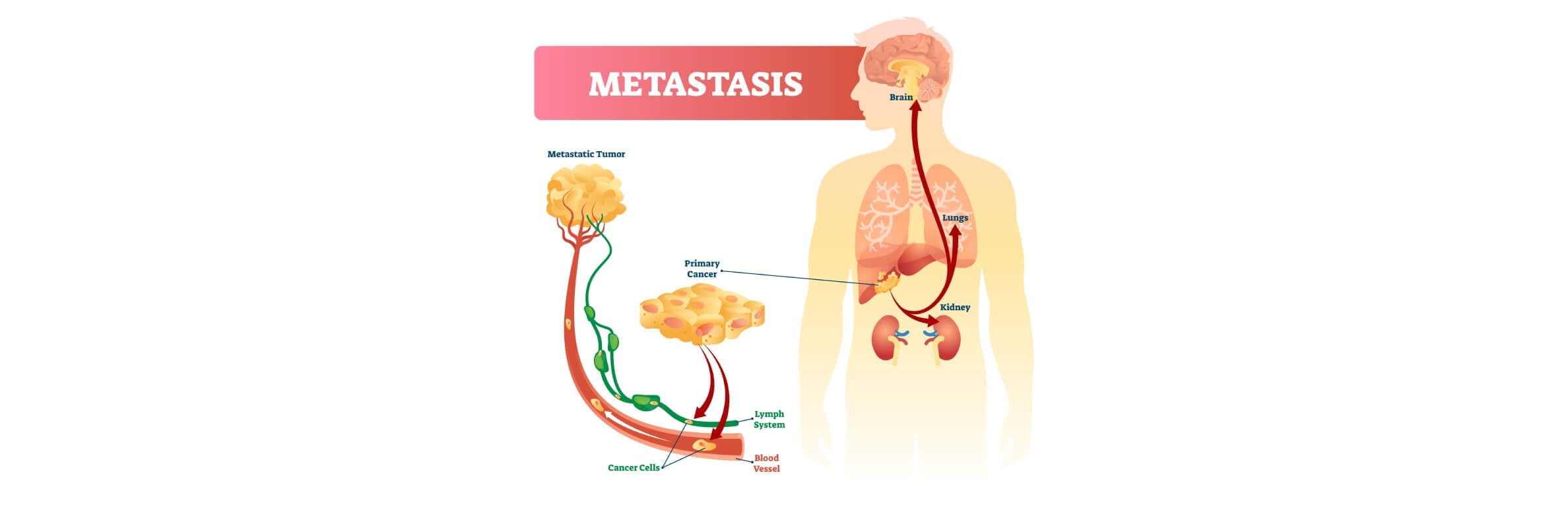
Метастазы в легких при раке молочной железы появляются, когда клетки рака молочной железы отделяются от первичной опухоли, попадают в кровоток или лимфатическую систему и оседают в легочной ткани, где начинают расти в виде вторичных опухолевых очагов. В настоящее время эффективное терапевтическое лечение такого метастатического заболевания по-прежнему остается серьезной клинической проблемой, что во многом обусловлено несовершенством методов ранней диагностики. Решающее значение для ранней диагностики, симптоматического лечения и прогнозирования состояния пациенток с метастазами рака груди в легкие имеет точное выявление процесса образования легочных микрометастазов на ранних стадиях развития клинически значимых легочных метастазов.
Что такое метастазы рака молочной железы в легкие
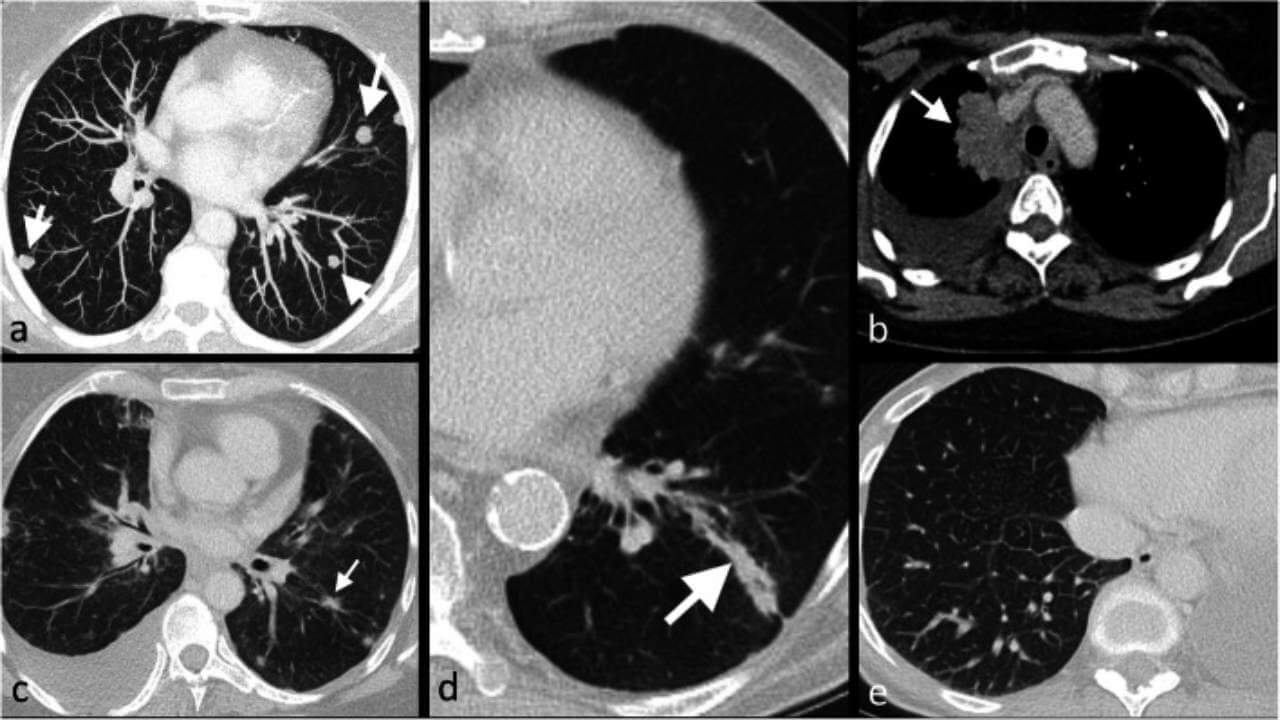
Метастазы в легких не являются раком легких – они состоят из клеток рака молочной железы. Чаще всего они появляются в виде множественных узлов различного размера, реже – в виде одиночного легочного узла. В большинстве случаев они не вызывают никаких симптомов и выявляются при проведении КТ (компьютерной томографии) грудной клетки.
Метастатическое заболевание характеризуется разнообразным клеточным составом с различными генетическими и фенотипическими свойствами, что приводит к различиям в темпах прогрессирования заболевания, метастазирования и развития резистентности к медикаментам. Так каков же механизм метастазирования рака в легкие? Рак груди – злокачественная опухоль, развивающаяся в тканях молочной железы. Опухоль образуется в результате процесса деления и размножения раковых клеток. По мере роста новообразования раковые клетки могут отделяться от первичной опухоли и распространяться на отдаленные органы или поражать близлежащие ткани.
Причины, по которым при первичном диагнозе рака молочной железы онкопроцесс часто метастазирует в легкие, до настоящего времени остаются предметом изучения. Однако результаты современных исследований демонстрируют, что важную роль в распространении метастазов играет взаимодействие между раковыми клетками и организмом человека, в частности, особенности легочной ткани, которые могут способствовать фиксации и росту опухолевых клеток. Существует несколько гипотез, объясняющих почему в одних органах метастазы появляются чаще, чем в других. Среди множества теорий медицинское сообщество считает наиболее достоверными две из них. Первая теория объясняет метастазирование тем, что для роста опухолевых клеток важна комбинация двух факторов: наличие самих раковых клеток и благоприятных условий для образования метастазов в конкретном органе. При наличии в органе благоприятных условий для фиксации и роста опухолевых клеток там могут образовываться метастазы. Напротив, при неблагоприятных условиях клетки не приживаются [4, 5]. Вторая теория основана на важной роли кровообращения: опухолевые клетки распространяются с кровотоком и оседают в тех органах, куда они проникают впервые. Легкие имеют ключевое значение в этом процессе, поскольку через них проходит большое количество венозной крови.
Симптомы метастатического рака молочной железы в легких
На ранних стадиях, когда очаги поражения небольшие, женщина может не ощущать никаких изменений в самочувствии. Легкие обладают значительным резервом, поэтому даже при наличии метастазов небольших размеров они могут продолжать нормально функционировать.
Как правило, симптомы появляются позже – когда метастазы увеличиваются в размерах или становятся более многочисленными. Тогда может появиться кашель, одышка, боль в груди или ощущение нехватки воздуха. Именно поэтому легочные метастазы часто выявляются во время плановых обследований, а не из-за жалоб пациентки.
Метастазы в легких могут проявляться такими симптомами:
- Постоянный или длительный кашель
- Боль или дискомфорт в груди
- Одышка или затрудненное дыхание
- Частые инфекции дыхательных путей
- Плевральный выпот – скопление жидкости между легким и грудной стенкой
Диагностика метастатического рака молочной железы в легких
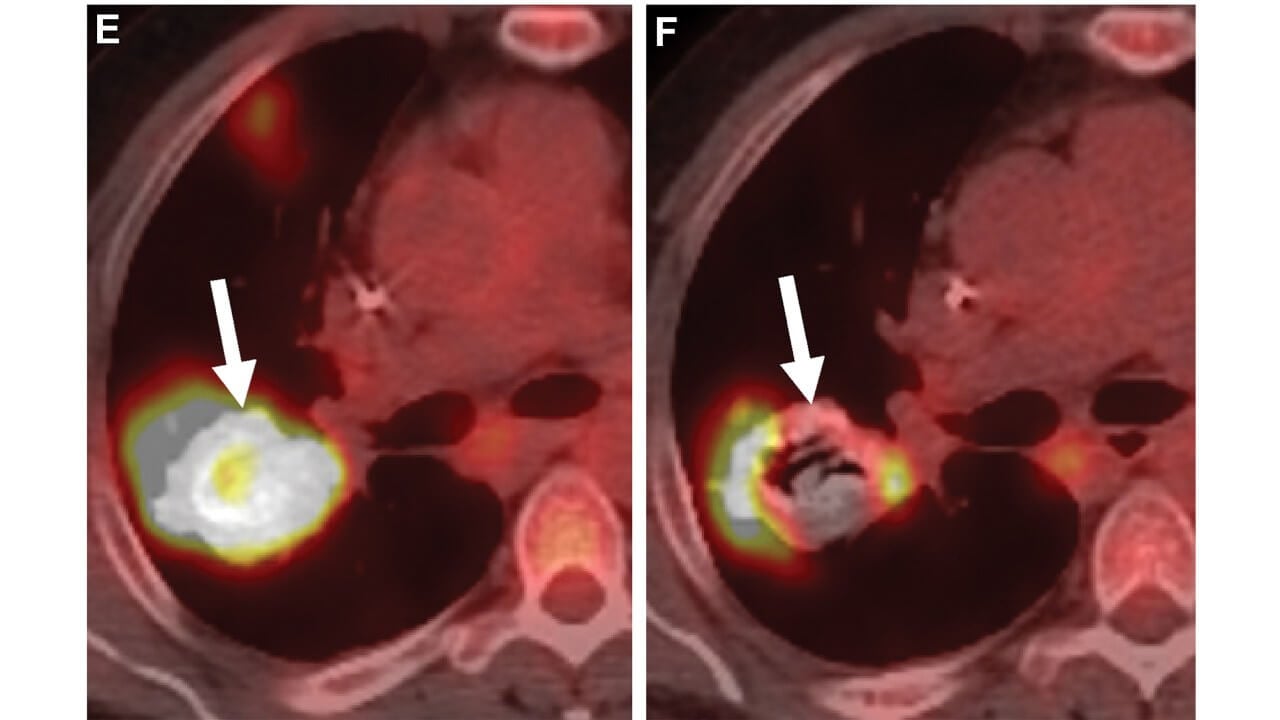
При подозрении на метастазы в легких часто назначают КТ или ПЭТ грудной клетки. Если по результатам визуализационного исследования врач выявляет опухоль и подтверждает, что она злокачественная, также важно установить, является ли новообразование первичным раком легких – опухолью, изначально развивающейся в легких, – или раком молочной железы, распространившимся на легкие. Лечение первичного рака легких отличается от лечения метастатического рака молочной железы, распространившегося на легкие.
Для подтверждения диагноза метастазов в легких проводятся такие исследования:
- Изучение образца мокроты под микроскопом
- Бронхоскопия – исследование ткани, а также, в некоторых случаях, взятие образца ткани из подозрительных участков путем введения гибкой трубки с источником света в дыхательные пути и легкие
- Пункционная биопсия легкого – взятие небольшого образца ткани путем введения иглы через кожу в пораженное легкое под контролем визуализации подозрительного участка
- Хирургическое удаление образца ткани из проблемного участка для последующего исследования
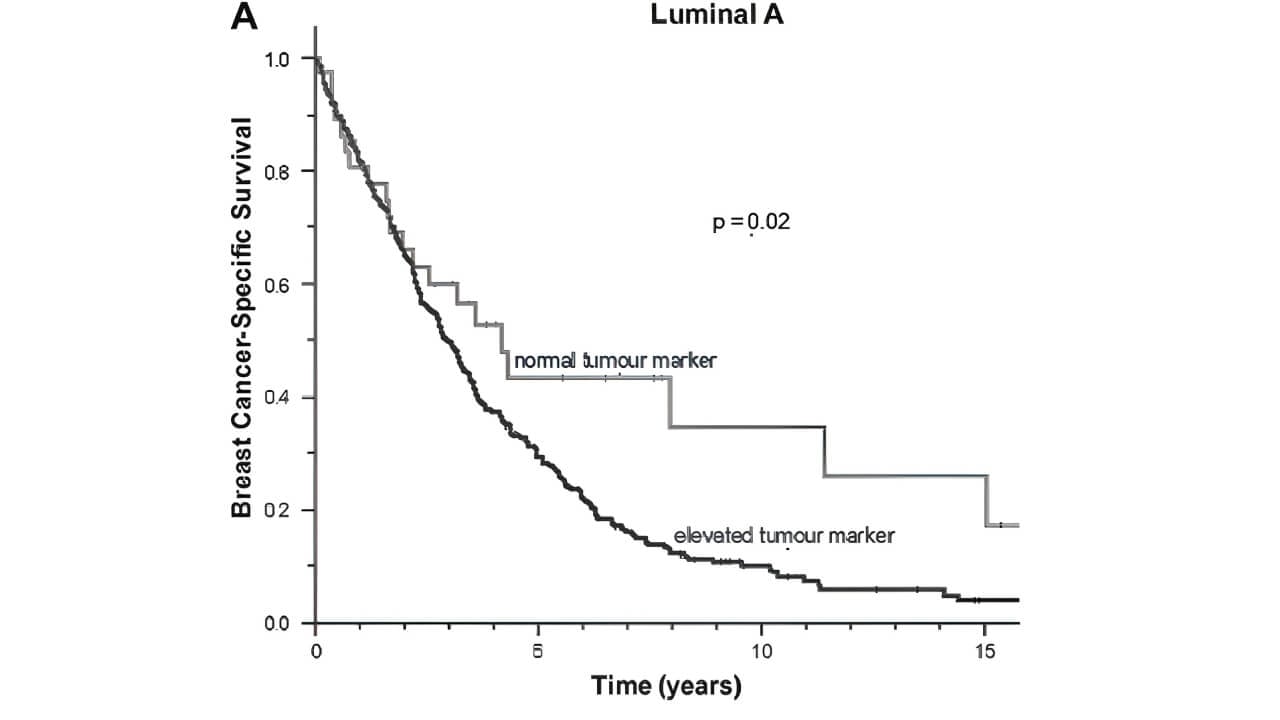
При ведении пациенток с карциномой молочной железы широко используются анализы крови на онкомаркеры – как при лечении метастатического заболевания, так и в комплексе с визуализационной диагностикой, сбором анамнеза и физическим обследованием. Уровень ракового антигена 15-3 (CA 15-3), ракового антигена 125 (CA 125) и карциноэмбрионального антигена (КЭА) повышается примерно в 80% и 40% случаев метастатического рака молочной железы соответственно [6]. В одном из исследований с участием пациенток с метастатическим раком молочной железы у некоторых женщин отмечался нормальный уровень CA 15-3, но повышенный уровень других онкомаркеров, в частности КЭА или CA 125. Подобное явление чаще наблюдалось при люминальных подтипах метастатического рака молочной железы, чем при более агрессивных трижды негативных формах заболевания [7].
Методы лечения метастазов в легких
Целью лечения метастазов в легких является облегчение симптомов, остановка или замедление прогрессирования метастазов в легких и обеспечение пациентке максимально возможного качества жизни. В международных протоколах метастатический рак рассматривается как системное заболевание, поэтому основу его лечения составляет системная терапия.
Системные методы лечения. Такая терапия воздействует на весь организм пациентки и является ключевым инструментом в борьбе с метастатическими опухолями в арсенале онкологов.
К системным методам лечения относятся:
- Гормональная терапия – проводится при гормонозависимых опухолях
- Химиотерапия – проводится при агрессивных или быстро прогрессирующих формах рака
- Таргетная терапия – проводится при наличии в новообразовании специфических молекулярных мишеней (например, HER2)
- Иммунотерапия при метастатическом раке груди – позволяет лечить рак в отдельных клинических случаях
Хирургическое лечение. Пациенткам с метастатическим раком молочной железы (МРМЖ) и метастазами в легких, отдельным пациенткам с раком молочной железы – с небольшим количеством поражений в легких, длительным безрецидивным периодом (ДБП) или гормон-рецептор-положительными опухолями – может помочь операция на легких для хирургического удаления метастазов в легких. Однако четких критериев отбора таких пациенток в настоящее время не существует [8].
Лучевая терапия. Данный метод подходит для лечения солитарных метастазов (СЛТТ – стереотаксическая лучевая терапия тела), проводится с целью облегчения симптомов, а также может быть показан при определенных осложнениях рака, например, сдавлении крупных кровеносных сосудов в грудной клетке.
Пациенткам важно знать не только о вариантах лечения метастазов рака груди в легкие, но и об ограничениях терапевтических возможностей. Многие методы лечения сопровождаются побочными эффектами: тошнотой, повышенной утомляемостью, выпадением волос, снижением иммунитета. Одним из главных недостатков методов лечения метастазов в легких является их ограниченная эффективность и, как правило, низкие показатели долгосрочной выживаемости – терапия не всегда позволяет полностью остановить развитие заболевания, во многих случаях обеспечивая лишь временный контроль над онкопроцессом.
Инновационные методы лечения
Терапия дендритными клетками
В 2011 году американский иммунолог Ральф Штейнман был удостоен Нобелевской премии за открытие дендритных клеток [9]. Опухолевые клетки возникают из нормальных клеток в человеческом организме, однако они могут проявлять определенную степень иммуногенности, при этом иммунная система обладает рядом механизмов, направленных на уничтожение опухолей. Поскольку дендритные клетки играют ключевую роль в функционировании иммунной системы и ее способности распознавать заболевания, ученые уверены, что их можно использовать для «укрепления» собственного иммунитета организма человека, чтобы он обрел способность более эффективно распознавать и уничтожать раковые клетки.
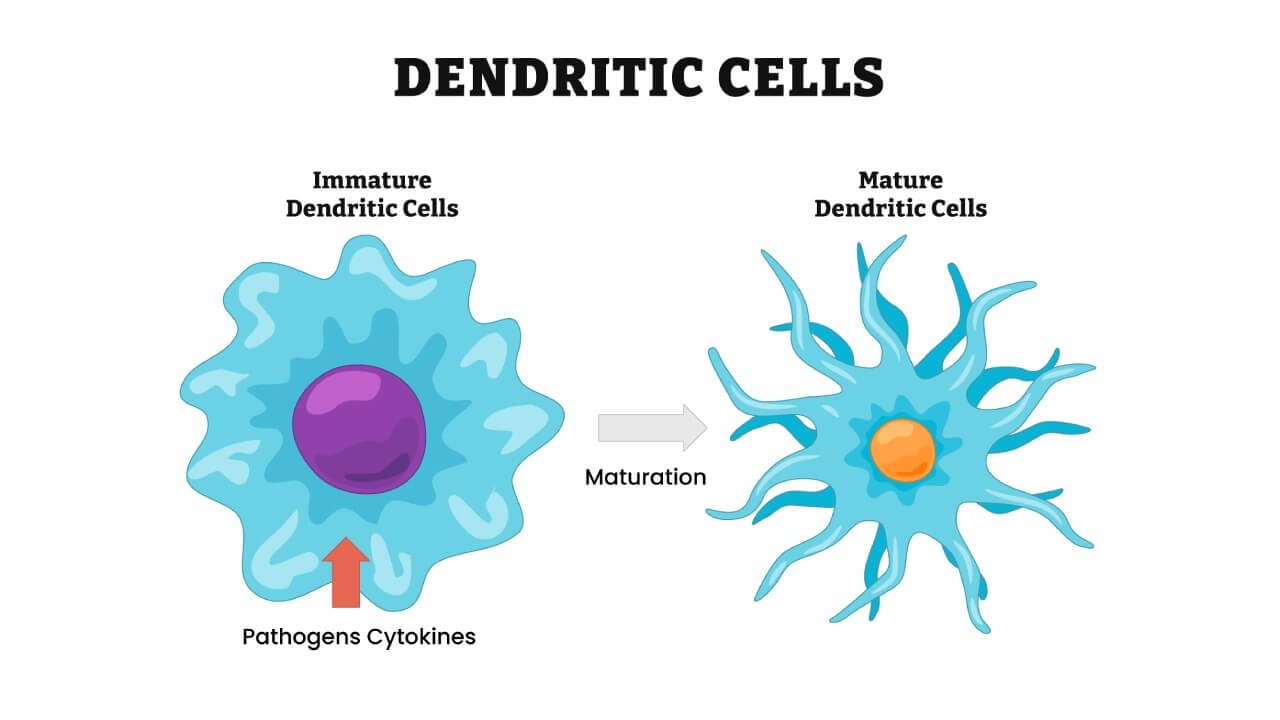
Дендритные клетки происходят из костного мозга и развиваются из миелоидных или лимфоидных предшественников. Они составляют менее 1% клеток в лимфоидных органах, а в других органах присутствуют еще реже [10]. Дендритные клетки являются ключевыми клетками иммунной системы. Их основная функция заключается в «обучении» иммунной системы распознавать раковые клетки. В рамках проведения терапии дендритными клетками осуществляется забор собственных дендритных клеток пациента, после чего в лабораторных условиях их активируют – «нагружают» опухолевыми антигенами и повторно вводят в организм онкобольного. В результате терапия стимулирует собственную иммунную систему пациентки уничтожать клетки рака молочной железы, включая метастазы в легких.
Такое лечение имеет особо важное значение при метастазах в легких, так как легкие являются иммунологически активным органом, а иммунный ответ в них часто подавляется опухолью. Активация иммунной системы может помочь добиться контроля над микрометастазами, которые не всегда отвечают на химиотерапию или лучевую терапию. Легкие, которые часто поражаются метастазами, обладают высокой иммунной активностью, но при этом склонны к формированию иммуносупрессивной среды. Это создает условия, при которых реактивация иммунного ответа посредством дендритных клеток патогенетически оправдана.
Эксклюзивное интервью с профессором Гансауге: дендритные клетки и их важная роль в стимуляции иммунной системы для борьбы с раком и старением
Неужели иммунная система может стать важнейшим инструментом для лечения рака и даже повлиять на процесс старения? Представляем вашему вниманию эксклюзивное интервью с профессором Гансауге – руководителем инновационной клиники по терапии дендритными клетками. В своем интервью специалист подробно рассказывает о принципах действия терапии дендритными клетками и объясняет, в каких случаях случаях такое лечение демонстрирует высокую эффективность, а также говорит о причинах, способствующих изменению нашего представления о современной медицине.
Терапия дендритными клетками – перспективный метод иммунотерапии для лечения метастазов в легких у пациенток с раком молочной железы, основанный на научно подтвержденных биологических принципах. Основная цель этого терапевтического подхода состоит не столько в быстром уменьшении опухолевой массы, сколько в восстановлении противоопухолевого иммунного контроля, особенно на ранних или бессимптомных стадиях метастатического процесса. На данном этапе терапию дендритными клетками при метастатическом раке молочной железы в легких следует рассматривать как дополнение к стандартному протоколу лечения в рамках клинических исследований или индивидуальных программ.
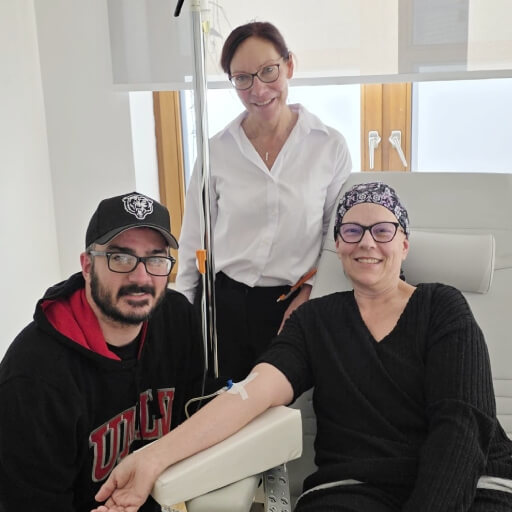
У Магдалены Ивановой из Болгарии диагностирован рак молочной железы IV стадии. Узнав о своем диагнозе, она начала искать дополнительные варианты лечения прогрессирующего рака груди. Внимание женщины привлекла терапия дендритными клетками. Магдалена обратилась в компанию Booking Health, специалисты которой помогли ей организовать лечение в Германии, где иммунотерапия проводится в комплексе со стандартными методами лечения. В своем интервью она делится личным опытом лечения прогрессирующего рака молочной железы.
Трансартериальная химиоэмболизация (ТАСЕ)
Химиоэмболизация при метастазах рака груди в легкие – это метод локорегиональной терапии, предполагающий введение химиотерапевтических препаратов непосредственно в артерии, питающие опухоль, с их одномоментной эмболизацией. Процедура обеспечивает:
- Более высокую локальную концентрацию лекарственных препаратов в онкологическом очаге
- Снижение системной токсичности лечения
- Ишемию опухолевой ткани
При химиоэмболизации легочной артерии эффективность лечения достигает 17%, тогда как при химиоэмболизации бронхиальной артерии, комбинированной эмболизации или химиоинфузии этот показатель повышается до 39%.
- Химиоэмболизация легочных артерий: процедура предполагает введение химиопрепаратов непосредственно в легочную артерию, питающую опухоль кровью, с одномоментной частичной окклюзией кровеносного сосуда (эмболизацией).
- Химиоэмболизация бронхиальных артерий: процедура предполагает введение химиопрепаратов в бронхиальную артерию, которая часто является источником кровоснабжения опухолей в легких.
- Эмболизация без введения химиопрепаратов (комбинированная эмболизация): в ходе процедуры выполняется лишь окклюзия сосудов, питающих опухоль.
- Химиоинфузия: процедура предполагает введение химиопрепаратов в артерию, питающую опухоль, без проведения эмболизации.
Лечение метастазов рака груди в легкие методом химиоэмболизации позволяет уничтожать крупные и многоочаговые легочные метастазы, в то числе метастатические поражения медиастинальных лимфатических узлов, у пациенток с ограниченными возможностями терапии. После процедуры TACE у пациенток не наблюдалось серьезных побочных эффектов. У женщин с химиорезистентными формами рака, не проходивших лечение другими методами, показатели метаболического ответа на терапию составили 40%. В отличие от печени, где по результатам ангиографии врачи могут констатировать гипер- или гиповаскулярные метастазы относительно нормальной ткани, метастазы в легких зачастую гиперваскулярны как по данным ангиографии бронхиальных, так и легочных артерий. Следовательно, внутриартериальное введение лекарственных препаратов при метастазах в легких обеспечивает хорошие терапевтические результаты [11].
Почему трансартериальная химиоэмболизация считается одним из наиболее эффективных методов в современной онкологии
Чтобы лучше разобраться в особенностях процедуры TACE, мы побеседовали с профессором Аттилой Ковачем – ведущим экспертом в области интервенционной радиологии с более чем 26-летним клиническим опытом. В своем интервью специалист подробно рассказывает о механизме действия TACE и о том, почему эта процедура стала «золотым стандартом» в области лечения опухолей высокой степени васкуляризации. Профессор Ковач также делится мнением о том, как малоинвазивные методы меняют подход к лечению рака, смещая акцент с радикальной терапии на паллиативную помощь.
Регионарная химиотерапия
Регионарная химиотерапия при раке груди с метастазами в легких представляет собой локорегиональный вид терапии, основанный на введении химиопрепаратов непосредственно в кровеносные сосуды, питающие опухоль. Процедура обеспечивает высокую концентрацию лекарственных препаратов в онкологическом очаге при минимальной системной токсичности лечения.
В рамках одного из исследований было установлено, что среди 162 пациенток, принимавших в нем участие, у 43 был диагностирован трижды негативный рак молочной железы 4 стадии с метастазами в легкие. Согласно данным этого исследования, у пациенток с ТНРМЖ в 40% случаев наблюдается возникновение легочных метастазов. Довольно часто эта группа онкобольных имеет противопоказания к хирургическому лечению и не отвечает на системную химиотерапию. В связи с этим женщинам проводилась изолированная торакальная перфузия (ИТП) – регионарный метод лечения, при котором кровоток в органах грудной клетки временно изолируется от системного кровотока с целью доставки чрезвычайно высоких доз химиопрепаратов непосредственно в легкие и средостение при минимизации системной токсичности лекарств. У пациенток с легочными метастазами трижды негативного рака молочной железы частота ответа на лечение составила 50%, тогда как медиана выживаемости повысилась до 14 месяцев с момента первой процедуры ИТП до последнего контакта с пациенткой [12].
В рамках другого исследования план лечения предполагал проведение внутриартериальной инфузии химиопрепаратов в сочетании с процедурой обратимой электропорацией: эти лечебные мероприятия были призваны обеспечить максимальную локальную концентрацию лекарственных препаратов в опухолевом очаге и достижение эффективного результата с минимальным количеством системных побочных эффектов. Обратимая электропорация – это инновационная процедура, при которой контролируемые электрические импульсы подаются непосредственно к опухолевой ткани, временно повышая проницаемость клеточных мембран. Специалистам удалось успешно применить эти методы лечения в комплексе на практике, обеспечив при этом хороший клинический ответ на лечение с минимальным профилем побочных действий. Через 2-7 дней после каждого из 21 циклов лечения во всех случаях, кроме одного, наблюдалось уменьшение размера новообразования. По результатам контрольных визуализационных исследований, проведенных через 4-8 недель после завершения курса терапии, врачи констатировали медианное уменьшение наибольшего диаметра опухоли на 45%, а также в двух случаях был достигнут полный ответ на лечение и в четырех – возможность проведения R0-резекции. Характерные для химиотерапии побочные эффекты отсутствовали или были минимальными. Легкая тошнота наблюдалась редко и обычно проходила в течение двух дней после сеанса лечения. Выпадение волос было зарегистрировано лишь в одном случае.
Такое лечение можно проводить повторно, при этом в отдельных случаях оно позволяет добиться резектабельности опухоли. Однако в определенных клинических ситуациях выполнение изолированной перфузии может оказаться более эффективным и безопасным вариантом лечения, поскольку эта процедура потенциально позволяет добиться полного уничтожения опухоли и снижения риска более агрессивного метастазирования рака [13].
Лечение за границей: сравнение стоимости медицинских процедур и терапевтических возможностей
В контексте планирования лечения метастазов в легких, возникших на фоне рака молочной железы, важным аспектом для пациенток и их семей является оценка финансовых затрат на терапию. Стоимость медицинских услуг может значительно варьироваться в зависимости от конкретной страны, особенностей действующей в этой стране системы здравоохранения, выбора методов лечения для пациенток с раком молочной железы (стандартных или инновационных) и необходимости применения индивидуальных или экспериментальных терапевтических подходов.
Ниже приведена сравнительная таблица с ориентировочной стоимостью основных методов лечения в четырех странах, считающихся популярными направлениями среди иностранных пациенток с раком молочной железы для медицинского туризма: Германии, Великобритании, США и Австралии. В этих странах находятся лучшие клиники для лечения рака груди с метастазами. Эта таблица поможет вам лучше оценить свой потенциальный бюджет и выбрать оптимальный вариант лечения с учетом ваших персональных потребностей и финансовых возможностей.
| Вид лечения | Стоимость в Германии | Стоимость в Великобритании | Стоимость в США |
|---|---|---|---|
| Хирургическое лечение | €25,000 – €45,000 | €35,000 – €55,000 | €65,000 – €85,000 |
| Химиотерапия | €80,000 – €150,000 за полный курс | €90,000 – €165,000 за полный курс | €100,000 – €180,000 за полный курс |
| Лучевая терапия | €28,000 – €42,000 | €35,000 – €65,000 | €40,000 – €80,000 |
| Гормональная терапия | €10,000 – €15,000 | €9,500 – €21,000 | €19,000 – €37,000 |
| Терапия дендритными клетками | €20,000 – €38,000 | Недоступна | €100,000 – €150,00 |
Современные подходы к лечению метастазов в легких при раке молочной железы: сравнительный анализ
Лечение метастазов в легких у пациенток с диагнозом метастатического рака молочной железы по-прежнему остается сложной клинической задачей, особенно при прогрессировании заболевания после стандартной системной терапии. Основу современных международных протоколов составляют традиционные методы лечения, включая системную химиотерапию, гормональную терапию и таргетную терапию, однако их эффективность нередко ограничивается развитием резистентности к лекарственным препаратам и системной токсичностью. В связи с этим акцент в клинической практике и исследовательских исследованиях все чаще смещается на инновационные и регионарные медицинские процедуры, направленные на повышение локального контроля над онкопроцессом, снижение системной нагрузки на организм и улучшение качества жизни пациенток.
Представляем вашему вниманию сравнительную таблицу с описанием стандартных и инновационных/экспериментальных методов лечения метастазов в легких от рака молочной железы с учетом их побочных эффектов и продолжительности курса терапии, а также свойственных им преимуществ и недостатков.
| Вид лечения | Показатели ответа на лечение | Показатели выживаемости | Побочные эффекты | Недостатки | Преимущества | Показания |
|---|---|---|---|---|---|---|
| Хирургическая процедура | Не проводится | ~70% на I стадии рака | Болевой синдром, риск заражения инфекцией, длительный период восстановления | 1. Риск развития осложнений (кровотечений, инфекций, побочных реакций на анестезию) 2. Длительный период восстановления и сроки госпитализации 3. Риск рецидива 4. Необходимость проведения дополнительных лечебных процедур | Полная хирургическая резекция опухоли, потенциально обеспечивающая излечение на ранних стадиях рака для пациенток, которые прошли лечение | Все локализованные опухоли |
| Химиотерапия | Менее 10% | ~20% на поздних стадиях рака | Тяжелые побочные эффекты (тошнота, выпадение волос) | 1. Системные побочные эффекты, низкое качество жизни во время лечения 2. Иммуносупрессия 3. Ограниченная эффективность при некоторых типах рака 4. Развитие резистентности с течением времени 5. Высокая частота рецидивов | Широко доступный метод, обеспечивающий эффективные результаты при системном заболевании. Временно замедляет рост опухоли | Злокачественные опухоли на всех стадиях |
| Лучевая терапия | Менее 15% | ~20% при локализованных формах рака | Повышенная утомляемость, раздражение кожи | 1. Локальные побочные эффекты, низкое качество жизни во время лечения 2. Побочные эффекты, проявляющиеся на конкретном участке тела (например, лучевой пневмонит) 3. Повышенный риск развития вторичных злокачественных новообразований после лечения 4. Недостаточная эффективность | Прицельно воздействует на очаг опухоли, позволяет уменьшить ее размер перед хирургическим удалением | Первичная опухоль и метастазы в головной мозг |
| Гормональная терапия | Менее 30% | ~25% на поздних стадиях рака | Умеренные побочные действия (приливы, увеличение веса, перепады настроения, снижение либидо) | 1. Снижение качества жизни во время лечения 2. Осложнения со стороны сердечно-сосудистой системы, нарушения обмена веществ, потеря плотности костной ткани, когнитивные и эмоциональные расстройства 3. Ограниченная продолжительность эффекта действия лечения, развитие гормональной резистентности с течением времени 4. Ограниченные показания – метод подходит только для лечения гормоночувствительных опухолей | Неинвазивный метод лечения с хорошей переносимостью, обеспечивающий долгосрочные результаты | Гормоночувствительные новообразования |
| Терапия дендритными клетками | 50-70% | ~65% | Минимальные побочные эффекты (гриппоподобные симптомы) | 1. Ограниченная доказательная база по сравнению с традиционными методами лечения 2. Персонализированное изготовление вакцин на основе дендритных клеток доступно только в специализированных центрах | Высокоспециализированный метод лечения, позволяющий сформировать пожизненный иммунитет против рака после всего одной инъекции вакцины, при этом сопровождается минимальными побочными эффектами и не повреждает здоровые клетки | Все злокачественные опухоли на всех стадиях |
| Трансартериальная химиоэмболизация | 40-50% | ~50% | Болевые ощущения, лихорадка, усталость | 1. Эффективность зависит от степени кровоснабжения опухоли (бронхиальные или легочные артерии) 2. Требует от врача высокого уровня квалификации в области интервенционной радиологии | Обеспечивает высокую локальную концентрацию лекарственных препаратов в опухоли и характеризуется минимальным профилем системных побочных эффектов | Неоперабельные метастазы в легких, прогрессирование заболевания после системной терапии |
| Регионарная химиотерапия | 30-50% | Не проводится | Локальный болевой синдром, кратковременная тошнота | 1. Проводится лишь в специализированных центрах 2. Ограниченная доступность и недостаточная база клинических данных | Помогает улучшить локальный контроль и облегчить симптомы, высокая локальная концентрация лекарственных средств | Химиорезистентные формы рака, неоперабельные метастазы в легких/td> |
Методы лечения метастазов в легких от рака груди в Германии
Германия занимает ведущие позиции среди стран, в которых пациентам предлагаются современные методы лечения рака. Этом способствует сочетание высокотехнологичной медицины, мощной научной базы и строгих стандартов качества лечения. В немецких клиниках придерживаются формата обслуживания онкобольных междисциплинарными командами врачей, что позволяет подбирать тактику лечения для каждой пациентки с учетом молекулярных характеристик опухоли и предшествующих линий терапии, особенно в сложных случаях распространения рака груди в легкие.
В этой стране пациенткам предоставляется доступ к современным системным препаратам, включая таргетную и иммунотерапию, а также к инновационным методикам локорегионального лечения, таким как высокоточная лучевая терапия (СЛТТ), интервенционные процедуры под визуальным контролем (TACE, регионарная химиотерапия, методы изолированной перфузии), электрохимиотерапия и персонализированные иммунотерапевтические подходы, в частности, терапия дендритными клетками.
Важным преимуществом медицины в Германии является практическое внедрение современных научных разработок в клиническую практику: лечение в этой стране основано на актуальных международных рекомендациях, передовых диагностических подходах и персонализированных программах ведения пациентов, что позволяет эффективно контролировать заболевание и поддерживать достойное качество жизни даже на поздних стадиях заболевания, в том числе при распространении рака груди в легкие.
Личный опыт лечения пациентки с рецидивом рака молочной железы и метастатическими очагами в легких
У Юлии сложный онкологический анамнез: рецидивирующий мультифокальный рак правой молочной железы (cT2N0, ER-положительный, HER2-отрицательный по данным ИГХ 2+), лечение гормональной терапией с октября 2023 года, а также рак легких IV стадии – аденокарцинома с мутацией в гене HER2 ex20ins и отрицательным статусом PD-L1.
Семья Юлии отмечает высокий уровень организации процесса лечения, поддержку со стороны координаторов и медицинской команды, а также комфортные условия пребывания в клинике, что помогает значительно уменьшить психологическое напряжение во время лечения. Благодаря профессиональному подходу профессора Гансауге и доктора Тауберта пациентка прожила на полтора года дольше, чем ей прогнозировали врачи на родине на момент постановки диагноза. По первоначальному прогнозу, озвученному онкологами женщине с диагностированным заболеванием в США, продолжительность жизни оценивалась примерно в шесть месяцев. Несмотря на распространение рака в легкие, у пациентки в настоящее время сохраняются хорошие показатели функционального состояния, физической активности и качества жизни. Семья выражает полное доверие к медицинской программе и команде специалистов, причастных к терапевтическому процессу, а также отмечает положительную динамику лечения:
«Условия пребывания в клинике комфортабельные, нет ощущения угрюмой больничной палаты. Напротив, здесь солнечно, красиво и по-домашнему уютно.
Благодаря блестящей работе и усердию профессора Гансауге и доктора Тауберта, моя мама прожила уже на полтора года дольше, чем предполагали врачи при первоначальном прогнозе. Я не являюсь квалифицированным специалистом по постановке диагнозов, но в глубине души знаю, что благодаря вам моя мама проживет еще тридцать лет, а, может, и еще дольше. И, повторюсь: врачи мамы в США утверждали, что ей осталось жить всего шесть месяцев... полтора года назад.
Кстати, она по-прежнему выглядит потрясающе: у нее густая красивая шевелюра рыжих волос, и талия у нее осталась такой же тонкой, как в подростковом возрасте. Несмотря на рак легких, она все еще почти каждое утро выходит на пробежку и выглядит так же хорошо, как и двадцать два года назад, когда я родился.
Ничего из этого не было бы возможно без опытной и замечательной команды медицинских специалистов, работающих в вашей компании. Я полностью доверяю предложенной вами программе и верю, что лечение будет и дальше приносить хорошие результаты».
Поездка на лечение за границу с Booking Health
Самостоятельный поиск наилучшей тактики лечения с учетом вашей индивидуальной клинической ситуации – довольно сложная задача. Испытав на себе многочисленные курсы лечения, проконсультировавшись со множеством специалистов и испробовав различные терапевтические процедуры, вам может быть трудно сориентироваться во всей предоставленной врачами информации. В таком случае пациенты зачастую выбирают первый же предложенный вариант лечения или соглашаются на лечение с применением стандартизированных терапевтических протоколов, которое повлечет за собой множество побочных эффектов, вместо того, чтобы рассмотреть возможность терапии с помощью инновационных процедур.
Если вы хотите сделать осознанный выбор и получить лечение рака в соответствии с индивидуально разработанной для вас схемой с учетом особенностей вашей конкретной клинической ситуации, проконсультируйтесь с медицинскими специалистами Booking Health. Компания Booking Health уже более 12 лет занимает ведущие позиции в сфере организации лечения за рубежом с применением новейших инноваций в медицине, поэтому ее специалисты обладают огромным опытом в составлении персонализированных комплексных программ лечения для каждого пациента. Booking Health пользуется репутацией авторитетной компании, которая предоставляет персонализированный подбор схемы лечения метастазов в легких при раке молочной железы и клиники с прямым бронированием приема в медицинском центре и полной поддержкой на каждом этапе лечения – от решения организационных вопросов до помощи в процессе лечения. Мы предлагаем:
- Оценку и анализ медицинских заключений пациентки
- Составление индивидуальной программы лечения
- Подбор подходящего медицинского учреждения для лечения
- Подготовку медицинской документации и ее направление в выбранную пациенткой для лечения клинику
- Консультации с врачами зарубежной клиники для разработки оптимальной медицинской программы на этапе подготовки к поездке на лечение
- Экспертные консультации во время пребывания в больнице
- Последующее консультирование пациентки после ее возвращения на родину по завершении медицинской программы
- Решение организационных вопросов в рамках подготовки к поездке на лечение за границу
- Координацию и организацию пребывания пациентки в другой стране
- Помощь в оформлении визы и бронировании авиабилетов
- Услуги переводчика и персонального координатора, который будет с вами на связи 24/7
- Прозрачные цены на лечение без скрытых платежей
Здоровье – главная ценность в жизни каждого человека, доверять заботу о которой стоит лишь лучшим специалистам с богатым опытом и проверенной репутацией. Booking Health – это ваш надежный партнер, который оказывает всестороннюю помощь на пути к восстановлению здоровья и улучшению качества жизни. Свяжитесь с медицинским консультантом компании, чтобы узнать больше о возможностях персонализированного лечения метастатического рака молочной железы у ведущих экспертов с использованием инновационных методов.
Инновации в онкологии: опыт пациентов Booking Health
Частые вопросы наших пациенток
Отправить запрос на лечениеМетастазы в легких – это вторичные новообразования в легких, которые образуются при распространении раковых клеток молочной железы из первичной опухоли в другие органы. Речь идет не о новом диагнозе «рак легких», а о проявлении распространенного рака груди.
Прогноз зависит от многих факторов: подтипа рака молочной железы (ER+, HER2+, трижды негативный), количества и размера метастазов рака груди в легкие, ответа на лечение и общего состояния пациентки. Современные методы лечения позволяют контролировать заболевание в течение многих лет и поддерживать достойное качество жизни.
Рак молочной железы распространяется на легкие, кости, печень, головной мозг, лимфатические узлы. В отдельных случаях поражаются сразу несколько органов.
Поражение легких является одним из наиболее распространенных вариантов метастазирования рака молочной железы. Согласно различным отчетам, метастазы в легких выявляют у 20-40% пациенток с метастатическими клетками рака молочной железы, особенно при агрессивных подтипах рака груди (трижды негативный рак молочной железы).
Клетки рака молочной железы попадают в кровоток или лимфатическую систему, проходят через сердце и оседают в мелких кровеносных сосудах легких, где при благоприятных условиях начинают расти и образовывать метастазы.
У пациенток наблюдаются такие симптомы: постоянный кашель, одышка, боль или давление в груди, повышенная утомляемость, рецидивирующие инфекции дыхательных путей, кровохарканье, плевральный выпот (скопление жидкости вокруг легких).
Да. На ранних стадиях или при метастазах в легких небольшого размера пациентки могут не испытывать никаких симптомов. Чаще всего их выявляют случайно во время КТ или ПЭТ. Именно поэтому регулярное прохождение контрольных визуализационных исследований после лечения рака молочной железы имеет такое важное значение.
При подозрении на метастазы в легких проводят КТ грудной клетки, ПЭТ-КТ, МРТ (в отдельных случаях), биопсию (для уточнения диагноза – при необходимости), молекулярно-генетические исследования, анализы крови на онкомаркеры и иммуногистохимический анализ.
Схема лечения всегда разрабатывается в индивидуальном порядке для каждой пациентки и может включать системную терапию (гормональную терапию, химиотерапию, таргетную терапию, иммунотерапию), лучевую терапию (включая СЛТТ), локорегиональные методы (химиоинфузию, химиоэмболизацию, изолированную торакальную перфузию), поддерживающую терапию на поздних стадиях рака и симптоматическое лечение.
Потенциально химиотерапия может обеспечить отличный результат лечения, но со временем ее эффективность снижается из-за развития резистентности к лекарственным препаратам. Такое лечение часто используют последовательно или в сочетании с другими видами терапии. Главная цель – добиться контроля над заболеванием и поддерживать достойное качество жизни пациентки.
Да, но не всем пациенткам. Иммунотерапия (особенно лечение ингибиторами контрольных точек иммунного ответа) применяется в зависимости от молекулярного подтипа опухоли, статуса PD-L1 и наличия специфических мутаций. Возможность проведения персонализированных иммунотерапевтических методов лечения, включая терапию дендритными клетками при метастазах рака груди в легкие, рассматривается в индивидуальном порядке.
Существуют ли в настоящее время инновационные или экспериментальные методы лечения метастазов в легких?
Да. К инновационным и экспериментальным методам относятся: ДКТ при метастатическом раке груди в легких (дендритно-клеточная терапия), регионарная химиотерапия, трансартериальная химиоэмболизация. Эти методы используются у отдельных пациенток и чаще всего сочетаются со стандартным лечением.
Германия славится своим высоким уровнем экспертного опыта в области онкологии, доступом к инновационным и экспериментальным медицинским программам, междисциплинарным подходом к лечению, услугами опытных специалистов, долгосрочными терапевтическими результатами и персонализированным высококачественным лечением рака.
Стоимость лечения зависит от конкретного вида терапии, продолжительности медицинской программы и использования в ходе лечебного процесса инновационных методов. В среднем расходы на лечение могут составлять от 20 до 40 тысяч евро, особенно при использовании экспериментальных или высокоспециализированных терапевтических процедур. Точная стоимость лечения определяется в индивидуальном порядке после анализа медицинской документации пациентки и с учетом цен на лечение рака за рубежом.
Показатели выживаемости могут существенно различаться: некоторые пациентки могут прожить всего несколько месяцев, а другие – еще много лет, особенно при хорошем ответе на лечение и применении современного комплексного подхода. На сегодняшний день метастатический рак молочной железы все чаще рассматривается как хроническое, поддающееся лечению заболевание, а не как смертный приговор.
Выбирайте лечение за рубежом и Вы, несомненно, получите отличный результат!
Авторы:
Статья составлена под редакцией экспертов в области медицины, врачей-специалистов доктора Надежды Иванисовой и доктора Дарьи Сухорученко. Для лечения состояний, о которых идет речь в статье, необходимо обратиться к врачу; информация в статье не предназначена для самолечения!
С редакционной политикой, которая отражает наше стремление к точности и прозрачности, можно ознакомиться здесь. Перейдите по ссылке, чтобы ознакомиться с нашими правилами.
Источники:
[1] Catarina Lourenço, Francisco Conceição, Carmen Jerónimo, Meriem Lamghari, Daniela M Sousa. Stress in Metastatic Breast Cancer: To the Bone and Beyond. Cancers (Basel). 2022 Apr 8;14(8):1881. doi: 10.3390/cancers14081881. [DOI] [PMC free article]
[2] H Kreisman, N Wolkove, H S Finkelstein, C Cohen, R Margolese, H Frank. Breast cancer and thoracic metastases: review of 119 patients. Thorax. 1983 Mar;38(3):175–179. doi: 10.1136/thx.38.3.175. [DOI] [PMC free article]
[3] Filippo Pesapane, Kate Downey, Anna Rotili, Enrico Cassano, Dow-Mu Koh. Imaging diagnosis of metastatic breast cancer. Insights Imaging. 2020 Jun 16;11:79. doi: 10.1186/s13244-020-00885-4. [DOI] [PMC free article]
[4] Jenny E Chu, Alison L Allan. The Role of Cancer Stem Cells in the Organ Tropism of Breast Cancer Metastasis: A Mechanistic Balance between the “Seed” and the “Soil”? Int J Breast Cancer. 2011 Nov 3;2012:209748. doi: 10.1155/2012/209748. [DOI] [PMC free article]
[5] Isaiah J Fidler. The pathogenesis of cancer metastasis: the 'seed and soil' hypothesis revisited. Nat Rev Cancer. 2003 Jun;3(6):453-8. doi: 10.1038/nrc1098. [DOI] [PubMed]
Смотреть больше
[6] C Tondini, D F Hayes, R Gelman, I C Henderson, D W Kufe. Comparison of CA15-3 and carcinoembryonic antigen in monitoring the clinical course of patients with metastatic breast cancer. Cancer Res. 1988 Jul 15;48(14):4107-12. [PubMed]
[7] R Yerushalmi, S Tyldesley, H Kennecke et al. Tumor markers in metastatic breast cancer subtypes: frequency of elevation and correlation with outcome. Ann Oncol. 2012 Feb;23(2):338-45. doi: 10.1093/annonc/mdr154. Epub 2011 May 4. [DOI] [PubMed]
[8] Junichi Soh, Yoshifumi Komoike, Tetsuya Mitsudomi. Surgical therapy for pulmonary metastasis of breast cancer. Transl Cancer Res. 2020 Aug;9(8):5044–5052. doi: 10.21037/tcr.2020.03.63. [DOI] [PMC free article]
[9] Roman Volchenkov, Florian Sprater, Petra Vogelsang, Silke Appel. The 2011 Nobel Prize in physiology or medicine. Scand J Immunol. 2012 Jan;75(1):1-4. doi: 10.1111/j.1365-3083.2011.02663.x. [DOI] [PubMed]
[10] C P Allan, C J Turtle, P N Mainwaring, C Pyke, D N J Hart. The immune response to breast cancer, and the case for DC immunotherapy. Cytotherapy. 2004;6(2):154-63. doi: 10.1080/14653240410005249. [DOI] [PubMed]
[11] F Edward Boas, Nancy E Kemeny, Constantinos T Sofocleous et al. Bronchial or Pulmonary Artery Chemoembolization for Unresectable and Unablatable Lung Metastases: A Phase I Clinical Trial. Radiology. 2021 Aug 31;301(2):474–484. doi: 10.1148/radiol.2021210213. [DOI] [PMC free article]
[12] Stefano Guadagni, Karl Aigner, Odisseas Zoras et al. Isolated thoracic perfusion in lung metastases from breast cancer: a retrospective observational study. Updates Surg. 2019 Mar;71(1):165-177. doi: 10.1007/s13304-018-00613-0. Epub 2018 Dec 12. [DOI] [PubMed]
[13] Kornelia Aigner, Emir Selak, Monika Pizon, Karl Reinhard Aigner. Arterial Infusion and Isolated Perfusion in Combination with Reversible Electroporation for Locally Relapsed Unresectable Breast Cancer. Cancers (Basel). 2024 Nov 28;16(23):3991. doi: 10.3390/cancers16233991. [DOI] [PMC free article]
Читайте:
Метастазы в легких: новейшие методы лечения и перспективные технологии
Комплексное руководство по лечению рака молочной железы 4 стадии: возможности терапии
Меню статьи:
- Что такое метастазы рака молочной железы в легкие
- Методы лечения метастазов в легких
- Инновационные методы лечения
- Лечение за границей: сравнение стоимости медицинских процедур и терапевтических возможностей
- Современные подходы к лечению метастазов в легких при раке молочной железы: сравнительный анализ
- Методы лечения метастазов в легких от рака груди в Германии
- Личный опыт лечения пациентки с рецидивом рака молочной железы и метастатическими очагами в легких
- Поездка на лечение за границу с Booking Health
- Частые вопросы наших пациенток
Не знаете, с чего начать?
Свяжитесь с Booking Health