Рак желчных протоков, также известный как холангиокарцинома, – это злокачественная опухоль, которая может развиваться в любой части желчевыводящей системы. Рак желчных протоков считается редким заболеванием по сравнению с другими видами рака. Ежегодно диагностируется менее 8000 случаев данной онкопатологии [1]. Заболевание чаще поражает мужчин, чем женщин. К сожалению, показатели выживаемости при раке желчных протоков довольно низкие: на 1 стадии заболевания выживаемость составляет около 20%, а на 4 стадии она снижается до 2-3%. Такое положение вещей свидетельствует о низкой эффективности современных протоколов диагностики и лечения.
В зависимости от локализации первичной опухоли различают внутрипеченочный рак желчных протоков (опухоль локализуется в мелких желчных протоках печени) и внепеченочный рак желчных протоков (перихилярный рак, опухоль Клацкина или рак дистальных отделов желчных протоков). Основываясь на этой классификации, проявления рака желчных протоков и подходы к его лечению могут несколько отличаться. Поздняя диагностика рака желчных протоков и неблагоприятный прогноз на прогрессирующей стадии этого заболевания сподвигли медицинское сообщество на поиски новых видов терапии, результатом которых стало открытие инновационных методов лечения.
Стадии заболевания и его клинические проявления
Для рака желчных протоков характерно бессимптомное течение до момента достижения опухолью местнораспространенной стадии, что является одной из главных сложностей в лечении данного онкологического заболевания. Независимо от локализации злокачественной опухоли, на ранних стадиях рака желчных протоков она обычно ограничена стенкой желчного протока и не распространяется на близлежащие кровеносные сосуды и лимфатические узлы. К сожалению, на этих стадиях редко присутствуют какие-либо проявления заболевания.
На 2 стадии рака желчных протоков происходит:
- Инвазия опухоли в печень или близлежащие жировые ткани (перихилярный рак)
- Прорастание опухоли в кровеносные сосуды или же наличие у пациента сразу двух опухолей (рак внутрипеченочных желчных протоков)
- Размер злокачественной опухоли достигает 12 мм или же есть признаки вовлечения в процесс 1-3 регионарных лимфоузлов (рак дистальных отделов желчных протоков)
На этой стадии у отдельных пациентов, особенно с раком внутрипеченочных желчных протоков и перихилярными опухолями, проявляются определенные симптомы: дискомфорт и тяжесть в правом подреберье, постоянная усталость, иногда также развивается желтуха. Как правило, рак желчных протоков 2 стадии выявляется случайно в ходе обследования, проводимого по другим причинам.
При раке желчных протоков 3 стадии, или местнораспространенном раке, злокачественная опухоль распространяется на окружающие ткани:
- Поражение онкопроцессом более 4 регионарных лимфоузлов или активная инвазия новообразования в регионарные кровеносные сосуды, например, верхнюю брыжеечную артерию и/или общую печеночную артерию (дистальная холангиокарцинома печени)
- Инвазия опухоли в основные кровеносные сосуды печени и/или их ветви с одной или обеих сторон, а также прорастание новообразования за пределы желчного протока с поражением 1-3 лимфоузлов в этой области (перихилярный рак желчных протоков)
- Проникновение злокачественных клеток в брюшину или другие близлежащие структуры (рак внутрипеченочных желчных протоков)
По данным специалистов, большинство случаев рака желчных протоков диагностируется именно на 3 стадии. Типичные симптомы включают тошноту, тупую боль в правом подреберье, желтуху, общее недомогание.
Как правило, на 4 стадии рака желчных протоков происходит распространение опухоли на отдаленные органы (дистальная и внутрипеченочная холангиокарцинома) или поражение более 4 лимфатических узлов в этой области. Помимо желтухи и других патологических проявлений на фоне нарушений функций печени и желчного пузыря у пациентов начинают проявляться симптомы, вызванные метастатическим поражением отдаленных органов. Они могут различаться в зависимости от того, в каком именно органе присутствуют метастазы.
Стандартные подходы к лечению рака желчных протоков
Тактика лечения рака желчных протоков определяется в зависимости от локализации опухоли и стадии заболевания [2]. К числу основных методов лечения холангиокарциномы печени относятся хирургия, химиотерапия и некоторые виды иммунотерапии.
Главным методом в протоколах лечения всех видов рака желчных протоков печени является хирургическое вмешательство. При внутрипеченочных опухолях обеспечение негативных краев резекции возможно при выполнении гемигепатэктомии, сегментэктомии, а также резекции желчных протоков в области бифуркации и внепеченочного желчного протока (у отдельных пациентов). Что касается лечения внепеченочных опухолей, в большинстве случаев требуется выполнение лобэктомии печени или резекции желчных протоков с регионарной лимфаденэктомией – зачастую в таких случаях хирургическое лечение выполняется без формирования постоянной стомы. Для лечения опухоли Клацкина (внутрипротоковой холангиокарциномы) или перихилярного рака проводится расширенная гепатэктомия с резекцией желчных протоков, после которой также может потребоваться выполнение реконструктивного вмешательства на воротной вене.
Основу лечения неоперабельного или метастатического рака желчных протоков составляет системная химиотерапия. Пациентам с этим заболеванием рекомендуется проведение неоадъювантной и адъювантной химиотерапии: неоадъювантная химиотерапия способна стимулировать ответ опухоли на лечение, поэтому она назначается пациентам с нерезектабельными опухолями, в то время как адъювантное химиотерапевтическое лечения обычно проводится после операции из-за высокого риска развития рецидива.
Иммунотерапия была включена в рекомендации по лечению рака желчных протоков совсем недавно. Согласно результатам исследований, ее проведение при этом заболевании способствует существенному повышение показателей общей выживаемости и беспрогрессивной выживаемости. Ингибиторы контрольных точке иммунного ответа также назначаются пациентам, у которых наблюдается прогрессирование рака после завершения первого курса лечения. Сочетание таргетной терапии ингибиторами контрольных точек иммунного ответа (ингибиторы PD-L1) и ингибиторами HER2 при HER2-положительных опухолях с системной химиотерапией помогает улучшить показатели общей выживаемости. Такое комбинированное лечение применяется при неэффективности терапии первой линии.
Инновации в лечении рака желчных протоков
Традиционные методы лечения применяются годами. Они помогли многим пациентам с раком желчных протоков, но сейчас врачи все чаще сталкиваются с резистентностью холангиокарциномы к терапии. К тому же системное лечение сопровождается выраженными побочными эффектами, из-за чего приходится прекращать терапию. В связи с этим были разработаны новые терапевтические методики, способствующие повышению эффективности лечения и улучшению качества жизни пациентов. Спектр инновационных видов терапии для лечения холангиокарциномы включает терапию дендритными клетками, трансартериальную химиоэмболизацию и методы интервенционной радиологии.
Терапия дендритными клетками
Терапия дендритными клетками является одним из видов иммунотерапии для лечения рака желчных протоков. В настоящее время проводятся множественные исследования, посвященные изучению эффективности метода при данном онкологическом заболевании. Дендритные клетки (ДК) – это тип специализированных иммунных клеток, способных распознавать злокачественные клетки и инициировать таргетный иммунный ответ против них. Таким образом, при проведении иммунотерапии обеспечивается таргетное уничтожение специфических раковых клеток без повреждения здоровых тканей. Терапия дендритными клетками стала революционным открытием в лечении рака, за которое Ральф Штайнман в 2011 году удостоился Нобелевской премии по физиологии и медицине [3].
Сегодня уже доступны результаты исследований, подтверждающие клиническую эффективность иммунотерапии в лечении неоперабельного или рецидивирующего рака желчных протоков. Вакцинация дендритными клетками – это персонализированная иммунотерапия, направленная на стимуляцию как врожденного, так и адаптивного иммунитета для борьбы с раком. Она зарекомендовала себя в качестве эффективного метода лечения холангиокарциномы. По данным исследований с участием 36 пациентов с холангиокарциномой, ранее перенесших хирургическое вмешательство, терапия дендритными клетками помогает замедлить прогрессирование заболевания. Другое исследование с участием пациентов с внутрипеченочной холангиокарциномой продемонстрировало улучшение показателей выживаемости и снижение вероятности развития рецидива, особенно при сочетании ДК с другими видами иммунотерапии или системного лечения.
Терапия дендритными клетками проводится на любой стадии заболевания, но чаще всего она назначается пациентам с поздними стадиями рака. Помимо обеспечения высокой частоты ответа на лечение при проведении в комбинации с традиционной терапией, вакцинация дендритными клетками обладает благоприятным профилем безопасности и, как правило, не вызывают серьезных побочных эффектов. Даже при проведении иммунотерапии дендритными клетками в сочетании с системными методами лечения, например, лучевой терапией, комбинированная терапия хорошо переносится пациентами и вызывает лишь незначительные побочные эффекты, в частности болевые ощущения.
Методы интервенционной радиологии
В настоящее время методы интервенционной радиологии становятся все более востребованными в лечении рака желчных протоков, поскольку они дают возможность обеспечить уничтожение опухоли малоинвазивным доступом без повреждения окружающих здоровых тканей. Чаще всего при борьбе с холангиокарциномой применяются термоабляция, криотерапия, электрохимиотерапия и артериальная эмболизация.
Термоаблация
Термоабляция – это интервенционная процедура, в ходе которой для точного уничтожения опухоли на нее воздействуют тепловой энергией. Различают два основных вида этой процедуры: радиочастотную абляцию (РЧА) и микроволновую абляцию (МВА). Оба метода в настоящее время включены в официальные протоколы лечения рака желчных протоков. Проведение РЧА и МВА показано пациентам с внутрипеченочной холангиокарциномой на ранней и промежуточной стадиях (I-II стадии), особенно при опухолях размером менее 3 см. По результатам ретроспективных исследований, при проведении термоабляции в комплексе с системной химиотерапией медиана общей выживаемости (ОВ) составляет 30-40 месяцев по сравнению с 12-18 месяцами при использовании лишь системной химиотерапии [4].
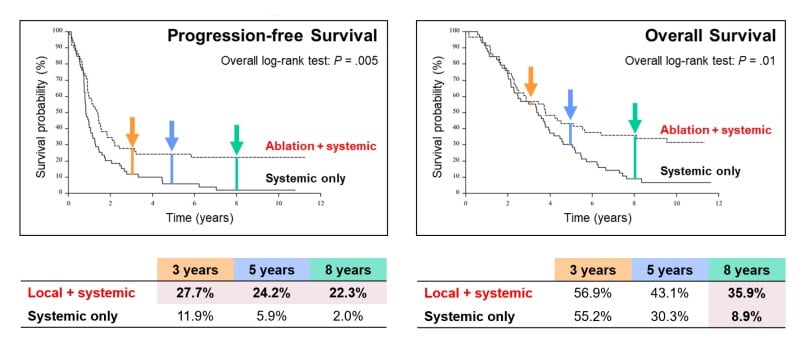
Источник: Ruers T et al. Локальное лечение нерезектабельных метастазов колоректального рака печени: результаты рандомизированного исследования II фазы. J Natl Cancer Inst. 2017 Sep 1;109(9)
Другое недавнее исследование продемонстрировало, что при проведении РЧА обеспечивается однолетняя и трехлетняя общая выживаемость в 82% и 47% случаев, соответственно, при этом у пациентов с единичными метастатическими поражениями отмечаются лучшие результаты лечения. Учитывая хорошие показатели локального контроля над опухолью и высокий профиль безопасности термоабляции, метод расценивается в качестве эффективного варианта лечения ранних стадий рака желчных протоков.
Криотерапия
Криоаблация – еще один инновационный вид терапии в арсенале современной медицины. Принцип действия данной процедуры основан на применении многократных циклов замораживания для достижения некроза опухоли [5]. Как правило, криоабляцию рекомендуют пациентам с ранними стадиями рака желчных протоков (I-II стадии) и солитарными опухолями. Следует отметить, что криоабляция применяется реже, чем термоабляция или трансартериальная химиоэмболизация, но эта процедура представляет собой потенциально более безопасный альтернативный вариант классической хирургической резекции, особенно если речь идет об опухолях с локализацией вблизи критически важных анатомических структур, поскольку в таких случаях термическое повреждение может представлять опасность для здоровья пациента. По результатам некоторых исследований, при проведении криоабляции в 70-80% случаев обеспечивается локальный контроль над опухолью, медиана беспрогрессивной выживаемости достигает 10 месяцев. Кроме того, криоабляция отличается исключительно низкой травматичностью, за счет чего обеспечивается быстрое восстановление пациента после процедуры и сокращение сроков пребывания в стационаре.
Электрохимиотерапия
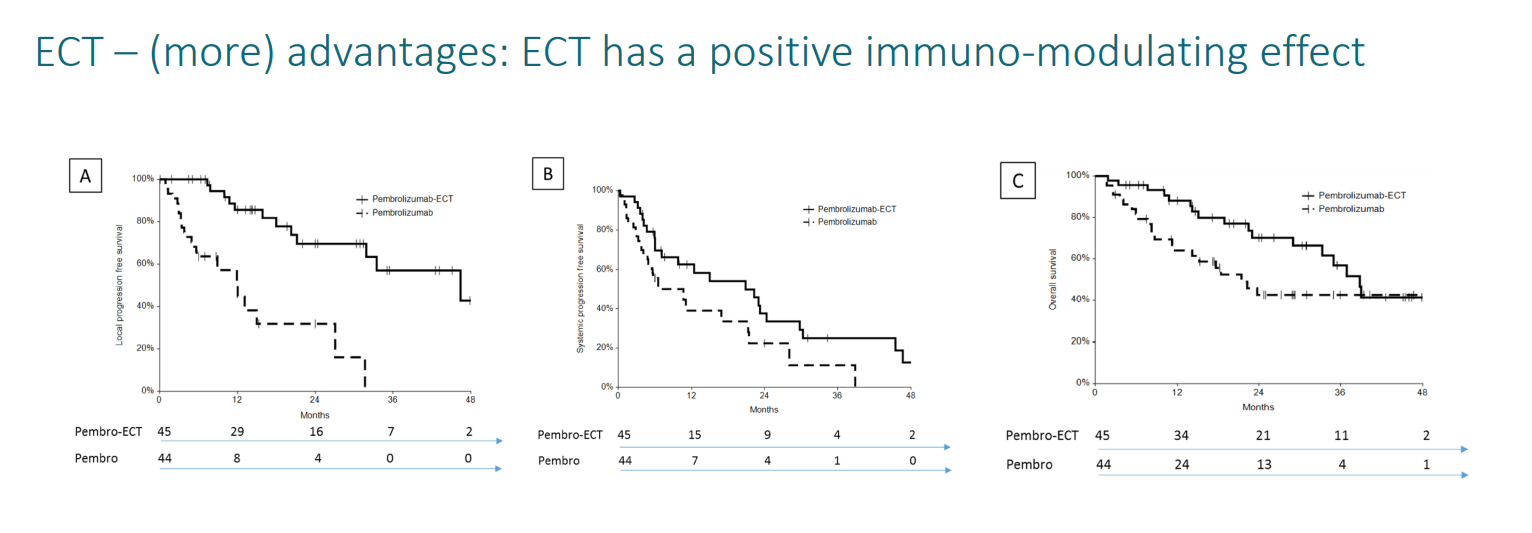
Электрохимиотерапия (ЭХТ) представляет собой малоинвазивный метод лечения, который в последнее время все чаще применяется при борьбе с раком желчных протоков [6]. Суть ЭХТ состоит в таргетном воздействии на опухоль электрическими импульсами для создания крошечных пор в мембранах злокачественных клеток, что способствует более избирательному и эффективному уничтожению новообразования химиопрепаратами. Метод пока находится на стадии клинических исследований, но он уже продемонстрировал многообещающие результаты в лечении неоперабельных и местнораспространенных холангиокарцином. Согласно данным исследований, включая исследование II фазы 2021 года, в 75-80% случаев был достигнут локальный контроль над заболевания, а медиана общей выживаемости составила до 17 месяцев, при этом такое лечение имеет минимальную системную токсичность. К тому же электрохимиотерапия отличается высокой эффективностью в лечении опухолей с локализацией вблизи крупных сосудов – проведение термоабляции в таких случаях сопряжено с рисками для здоровья пациента.
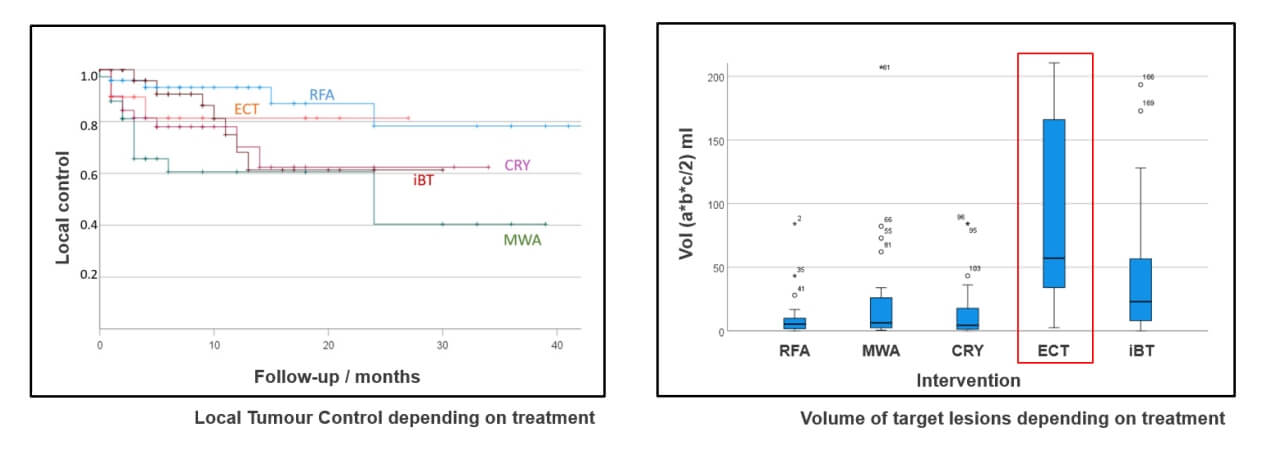
Источник: Kovács A et al. Долгосрочное сравнительное исследование локального контроля над опухолью при использовании различных техник абляции при первичных и вторичных злокачественных опухолях печени. J Pers Med. 2022 Mar 9;12(3):430
Проведение ЭХТ также способствует усилению эффекта от иммунотерапии за счет стимуляции иммунного ответа. В ходе нескольких исследований было зарегистрировано существенное улучшение показателей безрецидивной и общей выживаемости при сочетании ЭХТ с иммунотерапией. Такое комбинированное лечение демонстрирует большой потенциал в борьбе с местнораспространенным и даже метастатическим раком желчных протоков.
*Данные профессора, доктора медицины Аттилы Ковача
Региональная химиотерапия при раке желчных протоков
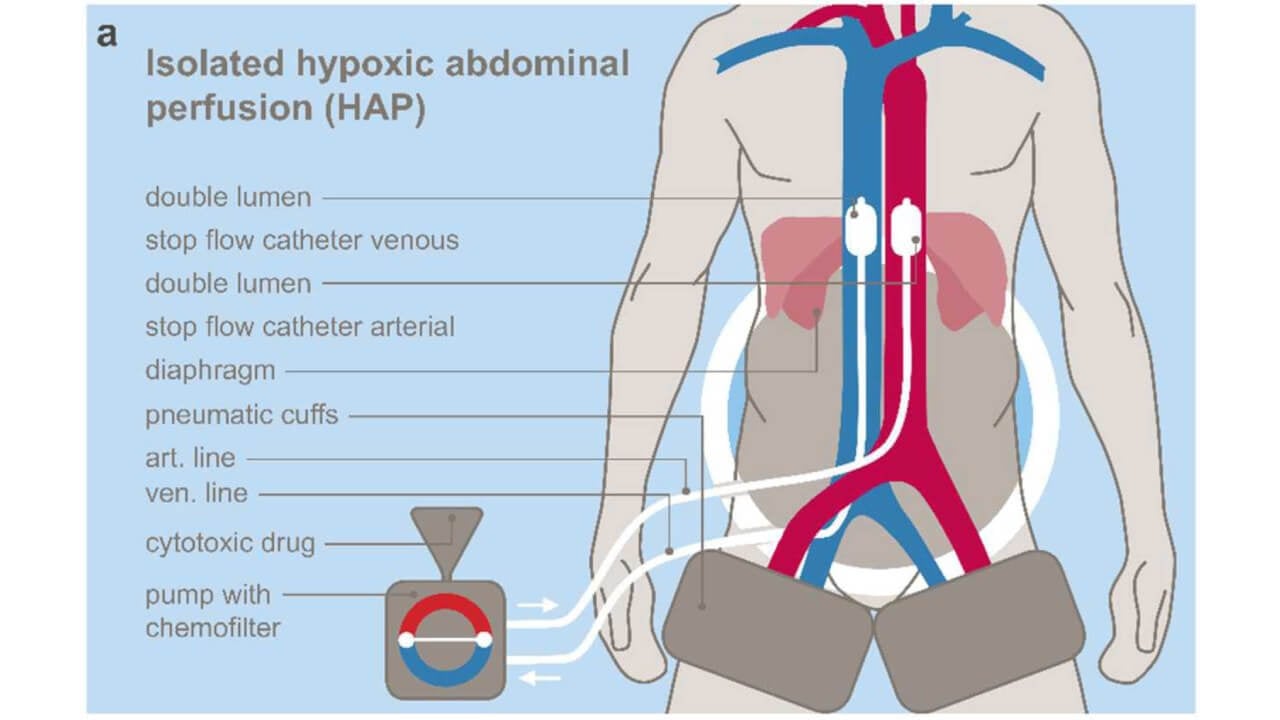
Регионарная химиотерапия при холангиокарциноме – важный метод лечения при метастазах и распространенном процессе. Химиопрепараты вводятся прямо в опухоль через артерии – с помощью гипоксической абдоминальной перфузии (HAP), верхней абдоминальной перфузии (UAP) и изолированной торакальной перфузии (ITP). Благодаря этому регионарная химиотерапия рака желчных протоков создает высокую концентрацию препаратов непосредственно в опухоли, при этом системная токсичность минимальна.
Профессор Карл Р. Айгнер с коллегами из клиники Онкологической клиники Медиас Бургхаузен разработали методику регионарной химиотерапии и доказали ее эффективность у пациентов с метастазами. Было проведено 189 циклов регионарной химиотерапии опухолей билиарного тракта с впечатляющими результатами: у 38% пациентов опухоль уменьшилась, у 41% онкологический процесс стабилизировался, а медиана выживаемости достигла 23 месяцев – это намного больше, чем при стандартном лечении.
Суть методики: кровоток изолируется в нужной области, и в этих условиях опухоль насыщается концентрированными химиопрепаратами, которые уничтожают раковые клетки. Параллельно химиофильтрация очищает венозную кровь до попадания препаратов в системный кровоток. Благодаря этом тяжелых осложнений лечения не было даже у ослабленных пациентов (ECOG 2-3).
Трансартериальная химиоэмболизация (TACE)
Трансартериальная химиоэмболизация (TACE) – малоинвазивный метод, который широко используется для лечения холангиокарциномы, особенно ее местнораспространенных форм и 4 стадии заболевания [7]. В ходе данной процедуры химиопрепараты вводятся непосредственно в опухоль, после чего с помощью эмболизирующего материала блокируется кровоснабжение новообразования. По результатам различных исследований, TACE помогает повысить показатели общей выживаемости, в некоторых случаях с 3,3 до 12,2 месяцев. Повышению эффективности TACE способствует проведение процедуры в комбинации с системными методами лечения, например, химиотерапией. Кроме того, трансартериальная химиоэмболизация обеспечивает более эффективные результаты по сравнению с традиционной поддерживающей терапией у пациентов с симптомами терминальной стадии рака, поскольку она способна улучшить общую выживаемость даже на этой стадии заболевания. Исследование с участием пациентов с нерезектабельным раком желчных протоков продемонстрировало, что 52,5% пациентов, прошедших трансартериальную химиоэмболизацию (TACE), были живы через 12 месяцев после лечения, по сравнению с 8,3% в группе, получавшей консервативное лечение. TACE обладает высоким профилем безопасности и обеспечивает низкую частоту интра- и послеоперационных осложнений, поэтому метод считается эффективной альтернативой системной химиотерапии в контексте лечения неоперабельных опухолей.
| Характеристики/Вид терапии | Показатели 2-летней выживаемости | Показатели ответа на лечение | Продолжительность курса лечения | Побочные эффекты |
|---|---|---|---|---|
| Стандартные методы лечения | ~25% на поздних стадиях рака | Менее 10% | Несколько циклов | Тяжелые побочные эффекты (тошнота, повышенная утомляемость, выпадение волос, иммуносупрессия, раздражение кожи) |
| Инновационные методы лечения | ~60% на поздних стадиях рака | 45-65% | До 4 сеансов | Незначительные побочные эффекты (дискомфорт в месте проведения лечебной манипуляции) |
*Данные Booking Health
Сравнительная таблица со стоимостью стандартных и инновационных методов лечения
| Метод лечения | Германия* | Великобритания | США |
|---|---|---|---|
| Стандартные методы лечения | €80 000 - €150 000 за полный курс | €90 000 - €165 000 за полный курс | €100 000 - €180 000 за полный курс |
| Инновационные методы лечения | €25 000 - €60 000 за полный курс | €70 000 - €120 000 за полный курс | €100 000 - €150 000 за полный курс |
*Цены могут отличаться в зависимости от применяемого вида терапии и продолжительности курса лечения, а также комбинации методов лечения в конкретном клиническом случае
История пациентки
Диагноз «рак желчных протоков» зачастую вызывает у пациента чувства отчаяния и безысходности. Традиционные методы лечения далеко не всегда обеспечивают эффективный результат, а побочные действия такой терапии еще больше ухудшают и без того не очень высокое качество жизнь онкобольного. Хедиджа на собственной шкуре испытала все это, но не опустила руки и решила пройти инновационное лечение рака желчных протоков.
В поисках альтернативного варианта лечения рака желчных протоков Хедиджа отправилась в Германию. Она знала, что эта страна занимает лидирующие позиции в сфере внедрения передовых технологий и новаторских методов лечения и что здесь ведут работу современные центры по лечению рака желчных протоков. Хедиджа получила консультацию одного из ведущих гастроэнтерологов Германии. Специалист по лечению рака желчных протоков в индивидуальном порядке составил для нее уникальную схему лечения. У Хедиджы наблюдалось прогрессирование симптомов, поэтому ей назначили трансартериальную химиоэмболизацию – малоинвазивный метод лечения, суть которого состоит в проведении регионарной химиотерапии с одномоментной блокировкой кровоснабжения опухоли. Поначалу Хедиджа переживала из-за предстоящей процедуры, поскольку ранее уже сталкивалась с изнурительными побочными эффектами химиотерапии. Врачи успокоили пациентку и заверили, что TACE в разы превосходит стандартную химиотерапию по эффективности, при этом процедура не вызывает системных побочных эффектов.
В конце концов, Хедиджа решилась на лечение с применением этого нового метода и осталась очень довольна результатом. «Врачи провели процедуру профессионально и она дала эффективный результат», – отмечает она. Благодаря быстрому ответу сотрудников компании Booking Health на запрос Хедиджы на лечение, организация ее поездки в Германию заняла всего одну неделю. При всесторонней поддержке со стороны Booking Health в организации и координации лечения в Германии у пациентки была возможность полностью сосредоточиться на своей терапии. Все организационные вопросы, включая трансфер и услуги переводчика, на себя взяла компания Booking Health, поэтому в ходе всей поездки Хедидже не нужно было беспокоится обо всех этих моментах. «Это был замечательный опыт», – говорит Хедиджа, подчеркивая важность сотрудничества с высококлассными экспертами в области медицинского туризма, такими как специалисты Booking Health, которые помогают получить лечение рака желчных протоков с применением инновационных методов.

Лечение рака желчных протоков на поздних стадиях – всегда есть шанс на успешный исход терапии
Диагноз «метастатический рак желчных протоков» – это серьезное испытание для пациента. Зачастую в такой ситуации человек испытывает чувство отчаяния и воспринимает свой диагноз как смертный приговор, особенно когда врачи говорят об ограниченных возможностях лечения на этой стадии заболевания. Однако даже при таком сложном диагнозе всегда есть надежда на благоприятный исход терапии, ведь современная медицина предлагает инновационные методы лечения, способные эффективно бороться с раком на поздних стадиях.
В наши дни медицина развивается стремительными темпами. Постоянно появляются инновационные разработки – от новаторских видов терапии и таргетных лечебных процедур до таких передовых технологий, как роботизированная хирургия. Традиционные методы лечения рака желчных протоков помогли многим пациентам, но, к сожалению, со временем они становятся менее эффективными, поскольку опухоли адаптируются к ним и становятся резистентными к терапии. К тому же при лечении по стандартному протоколу пациенты во многих случаях сталкиваются с серьезными побочными эффектами, требуются частые визиты в клинику и сложные терапевтические схемы, что может существенно повлиять на повседневную жизнь онкобольного. Многие пациенты испытывают физическое и эмоциональное истощение, что затрудняет поддержание достойного качества жизни и сохранение мотивации к лечению.
Именно в таких ситуациях важную роль приобретают инновационные методы лечения рака желчных протоков: иммунотерапия дендритными клетками, химиоэмболизация, интервенционные процедуры под визуальным контролем. Они действительно способны изменить прогноз пациента с раком поздней стадии. Эти терапевтические методики направлены не только на борьбу с прогрессированием заболевания, но и на укрепление иммунной системы и улучшение общего самочувствия пациента.
Обладая высокой эффективностью, инновационные методы лечения также отличаются простым проколом проведения и хорошей переносимостью. В отличие от традиционных системных видов терапии, многие из этих лечебных процедур выполняются амбулаторно, в большинстве случаев они предполагают минимальные сроки госпитализации, а также способствуют уменьшению количества и выраженности побочных эффектов. Инновационные методы лечения позволяют добиться контроля даже над терминальной стадией заболевания, обеспечивая эффективную борьбу с метастазами и замедление прогрессирования заболевания.
Сейчас онкологи располагают мощными инструментами, которые когда-то существовали лишь в теории. Если у вас или у кто-то из ваших близких диагностировали рак на поздней стадии, следует понимать, что возможности лечения рака желчных протоков 4 стадии существенно расширились, благодаря чему у онкобольного есть все шансы на достижение хороших результатов и увеличение продолжительности жизни. Поэтому не стоит упускать шанс получить лечение с применением инновационных методов с научно доказанной эффективностью, которое способно подарить новую надежду.
Поездка на лечение за границу с Booking Health
Самостоятельный поиск наилучшей тактики лечения с учетом вашей индивидуальной клинической ситуации – довольно сложная задача. Испытав на себе многочисленные курсы лечения, проконсультировавшись со множеством специалистов и испробовав различные терапевтические процедуры, вам может быть трудно сориентироваться во всей предоставленной врачами информации. В таком случае пациенты зачастую выбирают первый же предложенный вариант лечения или соглашаются на лечение с применением стандартизированных терапевтических протоколов, которое повлечет за собой множество побочных эффектов, вместо того, чтобы рассмотреть возможность терапии с помощью инновационных процедур.
Если вы хотите сделать осознанный выбор и получить лечение рака в соответствии с индивидуально разработанной для вас схемой с учетом особенностей вашей конкретной клинической ситуации, проконсультируйтесь с врачами-консультантами Booking Health. Компания Booking Health уже более 12 лет занимает ведущие позиции в сфере организации лечения за рубежом с применением новейших инноваций в медицине, поэтому ее специалисты обладают огромным опытом в составлении персонализированных комплексных программ лечения. Booking Health пользуется репутацией авторитетной компании, которая предоставляет персонализированный подбор схемы лечения рака желчных протоков 4 стадии и клиники с прямым бронированием приема в медицинском центре и полной поддержкой на каждом этапе лечения – от решения организационных вопросов до помощи в процессе лечения. Мы предлагаем:
- Оценку и анализ медицинских заключений пациента
- Составление индивидуальной программы лечения
- Подбор подходящего медицинского учреждения для лечения
- Подготовку медицинской документации и ее направление в выбранную пациентом для лечения клинику
- Консультации с врачами зарубежной клиники для разработки оптимальной медицинской программы на этапе подготовки к поездке на лечение
- Экспертные консультации во время пребывания в больнице
- Последующее консультирование пациента после его возвращения на родину по завершении медицинской программы
- Решение организационных вопросов в рамках подготовки к поездке на лечение за границу
- Координацию пребывания пациента в другой стране, помощь в бронировании отеля или апартаментов на период лечения
- Помощь в оформлении визы и бронировании авиабилетов
- Услуги переводчика и персонального координатора, который будет с вами на связи 24/7
- Прозрачные цены на лечение без скрытых платежей
Здоровье – главная ценность в жизни каждого человека, доверять заботу о которой стоит лишь лучшим специалистам с богатым опытом и проверенной репутацией. Booking Health – это ваш надежный партнер, который оказывает всестороннюю помощь на пути к восстановлению здоровья и улучшению качества жизни. Свяжитесь с врачом-консультантом компании, чтобы узнать больше о возможностях персонализированного лечения метастатического рака желчных протоков у ведущих экспертов с использованием инновационных методов.
Современная онкология: опыт пациентов Booking Health
Частые вопросы о лечении рака желчных протоков
Отправить запрос на лечениеК числу наиболее эффективных методов лечения рака желчных протоков относятся хирургическая резекция (при резектабельном раке), химиотерапия, таргетная терапия (например, ингибиторы FGFR, направленные на специфические мутации в генах) и иммунотерапия. Выбор метода лечения зависит от стадии, локализации и молекулярного профиля опухоли.
К сожалению, холангиокарцинома поддается полному излечению лишь на ранних стадиях. Для обеспечения куративного лечения требуется проведение операции, результатом которой станет полное удаление опухоли с отрицательными краями резекции. На поздних стадиях онкологического заболевания или при наличии метастазов пациентам назначают паллиативное лечение, направленное на продление жизни и облегчение симптомов.
Общая пятилетняя выживаемость при ранних стадиях рака составляет около 20-25%. При метастатическом раке показатель пятилетней выживаемости составляет менее 5%.
Необходимый пациенту комплекс исследований определяется в зависимости от присутствующих у него симптомов и их выраженности. Качество диагностики также зависит от уровня медучреждения, в котором будет проходить обследование. Как правило, проводятся:
- Визуализационные исследования (МРТ/МРХПГ, КТ, УЗИ)
- Анализы крови на онкомаркеры (CA 19-9, CEA)
- Биопсия (эндоскопическая или чрескожная)
Эндоскопическая ретроградная холангиопанкреатография (ЭРХПГ) и холангиоскопия проводятся как с целью постановки диагноза, так и для определения стадии рака желчных протоков.
На ранних стадиях заболевание часто протекают бессимптомно, но иногда все же может проявляться легкой болью в животе или нарушением уровня печеночных ферментов.
На поздних стадиях при раке желчных протоков развивается желтуха, моча становится темной, а стул светлым, появляется зуд, наблюдается потеря веса и повышенная утомляемость из-за обструкции желчных протоков и поражения печени.
Холангиокарцинома считается агрессивной опухолью, но в некоторых случаях она прогрессирует относительно медленно. Данный вид рака часто распространяется на печень, лимфатические узлы и брюшину. Во многих случаях на начальных стадиях онкологическое заболевание протекает практически бессимптомно, чем и объясняется его поздняя диагностика.
Как правило, прогноз при раке желчных протоков 4 стадии неблагоприятный. Медиана выживаемости обычно составляет 6-12 месяцев. Лечение на этой стадии направлено на контроль симптомов и улучшение качества жизни. Включение в схему лечения инновационных видов терапии способно несколько увеличить продолжительность жизни у отдельных пациентов.
Да, хирургическое вмешательство является основным методом лечения, потенциально обеспечивающим излечение рака желчных протоков на ранних стадиях. В зависимости от локализации опухоли, хирурги проводят резекцию печени или операцию Уиппла. Решение о целесообразности проведения хирургического вмешательства принимается с учетом размера опухоли, степени распространения онкопроцесса и функции печени.
Да, к ним относятся иммунотерапия (вакцинация дендритными клетками, лечение ингибиторами PD-1) и методы интервенционной радиологии (термоабляция, криоабляция). В клинических испытаниях активно изучаются новые таргетные препараты и комбинированные методы лечения для борьбы с раком желчных протоков.
В зависимости от эффективности паллиативного лечения и общего состояния здоровья пациента ожидаемая продолжительность жизни составляет от нескольких месяцев до одного года. При купировании симптомов ключевую роль играет поддерживающая терапия.
Факторы риска развития рака желчных протоков:
- Первичный склерозирующий холангит (ПСХ)
- Хроническое воспаление желчных протоков
- Фасциолез
- Кисты холедоха
- Гепатит B/C
- Цирроз печени
Развитие онкопатологии также может быть связано с воздействием таких модифицируемых факторов окружающей среды, как курение и употребление определенных продуктов питания. Из рациона питания следует исключить сырые морепродукты и грибы, поскольку они повышают риск заражения специфической паразитарной инфекцией желчных протоков. Согласно статистическим данным, эта инфекция связана с более высокой частотой развития рака желчных протоков в Азии. Тем не менее, в большинстве случаев точно установить причину развития онкологического заболевания невозможно.
Как правило, нет. Большинство случаев рака желчных протоков возникают спорадически – без очевидной причины или наследственной предрасположенности. Тем не менее, такие генетические заболевания, как синдром Линча и мутации гена BRCA, все же способствуют повышению риска развития этого онкологического заболевания.
Внутрипеченочный рак развивается в желчных протоках внутри печени.
Внепеченочный рак развивается в желчных протоках за пределами печени – перихилярная холангиокарцинома (опухоль Клацкина) и рак дистальных отделов желчных протоков. Локализация опухоли определяет профиль симптомов, тактику лечения и прогноз пациента.
Пациенты с таким диагнозом могут получить высококлассную медицинскую помощь в крупных центрах, специализирующихся на лечении рака желчных протоков, которые обладают экспертным опытом в области гепатобилиарной хирургии и онкологии. К числу таких медучреждений относятся:
- Онкологический центр им. М. Д. Андерсона
- Мемориальный онкологический центр имени Слоуна-Кеттеринга
- Университетская клиника Мюнхенского университета им. Людвига-Максимилиана
- Клиника Гелиос Берлин-Бух
Выбирайте лечение за рубежом и Вы, несомненно, получите отличный результат!
Авторы:
Статья составлена под редакцией экспертов в области медицины, врачей-специалистов доктора Надежды Иванисовой и доктора Богдана Михальнюка. Для лечения состояний, о которых идет речь в статье, необходимо обратиться к врачу; информация в статье не предназначена для самолечения!
С редакционной политикой, которая отражает наше стремление к точности и прозрачности, можно ознакомиться здесь. Перейдите по ссылке, чтобы ознакомиться с нашими правилами.
Источники:
[1] American Cancer Society. Key Statistics for Bile Duct Cancer. https://www.cancer.org/cancer/types/bile-duct-cancer/about/key-statistics.html
[2] NIH, National Cancer Institute. Bile Duct Cancer Treatment. https://www.cancer.gov/types/liver/bile-duct-cancer/treatment
[3] ARoman Volchenkov, Florian Sprater, Petra Vogelsang, Silke Appel. The 2011 Nobel Prize in physiology or medicine. Scand J Immunol. 2012 Jan;75(1):1-4. doi: 10.1111/j.1365-3083.2011.02663.x. [DOI] [PubMed]
[4] Theo Ruers, Frits Van Coevorden, Cornelis J A Punt et al. Local Treatment of Unresectable Colorectal Liver Metastases: Results of a Randomized Phase II Trial. J Natl Cancer Inst. 2017 Sep 1;109(9):djx015. doi: 10.1093/jnci/djx015. [DOI] [PubMed]
[5] Journal of Vascular and Interventional Radiology. Image-Guided Ablation of Recurrent or Unresectable Intrahepatic Cholangiocarcinoma. https://www.jvir.org/article/S1051-0443(23)00194-X/abstract
[6] European Review for Medical and Pharmacological Sciences. Electrochemotherapy of cholangiocellular carcinoma at hepatic hilum: a case report. https://www.europeanreview.org/wp/wp-content/uploads/7051-7057.pdf
[7] Joseph J Zechlinski, William S Rilling. Transarterial Therapies for the Treatment of Intrahepatic Cholangiocarcinoma. Semin Intervent Radiol. 2013 Mar;30(1):21–27. doi: 10.1055/s-0033-1333650 [DOI] [PMC free article]
[8] Yogesh Vashist, Kornelia Aigner, Sabine Gailhofer and Karl R. Aigner. Therapeutic Effect of Regional Chemotherapy in Diffuse Metastatic Cholangiocarcinoma. Cancers 2022, 14(15), 3701; https://doi.org/10.3390/cancers14153701. [DOI]
Читайте:
Опухоль Клатскина: лечение рака желчных протоков в Германии
Меню статьи:
- Стадии заболевания и его клинические проявления
- Стандартные подходы к лечению рака желчных протоков
- Инновации в лечении рака желчных протоков
- Сравнительная характеристика методов лечения
- История пациентки
- Лечение рака желчных протоков на поздних стадиях – всегда есть шанс на успешный исход терапии
- Поездка на лечение за границу с Booking Health
- Частые вопросы о лечении рака желчных протоков
Не знаете, с чего начать?
Свяжитесь с Booking Health