Рак эндометрия – это наиболее распространенное гинекологическое злокачественное заболевание в странах Европейского Союза. По данным Европейской системы информации о раке (ECIS) [1], и Европейской сети канцер-регистров (ENCR) [2], в 2022 году в Европе было диагностировано около 125 000 новых случаев рака эндометрия, что составляет почти 6% всех случаев рака у женщин в регионе.
Заболевание преимущественно поражает женщин в постменопаузе: средний возраст пациенток на момент постановки диагноза составляет около 67 лет. Довольно часто рак матки выявляют на ранних стадиях, в основном благодаря таким симптомам, как постменопаузальные кровотечения. Тем не менее, частота заболеваемости постепенно растет. Согласно данным Европейского общества медицинской онкологии (ESMO), такая неблагоприятная тенденция в значительной степени обусловлена ростом уровня ожирения и старением населения. [3]
Общая информация о раке эндометрия
Рак эндометрия является наиболее распространенным злокачественным заболеванием женской репродуктивной системы в Европе, которое преимущественно диагностируется у женщин после наступления менопаузы. Ввиду неуклонного роста заболеваемости этот вид рака становится все более серьезной проблемой для общественного здравоохранения.
Гистологические типы рака эндометрия
Существует два основных типа рака эндометрия:
- Опухоли I типа (эндометриоидные аденокарциномы) являются более распространенной и менее агрессивной формой рака матки. Это эстрогензависимые новообразования, развитие которых часто связано с такими факторами риска, как ожирение, сахарный диабет и неконтролируемое воздействие эстрогенов. Как правило, опухоли типа I растут медленно и диагностируются на ранней стадии.
- Опухоли II типа (неэндометриоидный рак) включают серозные, светлоклеточные и другие редкие гистологические типы рака матки. Эта группа новообразований не является эстрогензависимой, чаще характеризуется высокой степенью злокачественности и агрессивным течением, а также диагностируется на поздних стадиях.
Клинические стадии рака матки и их роль в выборе тактики лечения
Для определения стадии рака эндометрия используется система FIGO, служащая основой для выбора оптимальной тактики лечения:
- Стадия I – онкопроцесс не выходит за пределы матки.
- Стадия II – опухоль распространяется на строму шейки матки, но все еще локализуется в пределах матки.
- Стадия III – заболевание распространяется за пределы матки, поражая близлежащие ткани или лимфатические узлы.
- Стадия IV – рак распространяется на отдаленные органы: мочевой пузырь, кишечник или легкие.
Точное определение стадии рака эндометрия играет решающую роль в выборе наилучшей тактики лечения. Во многих случаях на ранних стадиях достаточно проведения хирургического вмешательства по удалению опухоли, тогда как на поздних стадиях для улучшения терапевтических результатов могут потребоваться дополнительные лечебные мероприятия, например, лучевая терапия или химиотерапия.
Стандартные подходы к лечению рака эндометрия
Как правило, врачи подбирают оптимальный комплекс лечебных мероприятий, исходя из диагностированной у пациентки стадии рака эндометрия, что обеспечивает персонализированный подход к терапии. При лечении рака матки на 0 стадии, когда предраковые изменения присутствуют лишь во внутренней оболочке матки, рассматривается возможность проведения гормональной терапии или малоинвазивного хирургического вмешательств, особенно если женщина желает сохранить репродуктивную функцию.
Стандартным подходом к лечению рака матки 1 стадии, особенно рака эндометрия 1а стадии, является хирургическое удаление матки, маточных труб и яичников (тотальная гистерэктомия с двусторонней сальпингоофорэктомией). При применении такой тактики лечения врачам удается не только обеспечить полное удаление опухоли, но и с максимальной точностью определить стадию новообразования. Большинство пациенток с раком матки 1 стадии все чаще отдают предпочтение малоинвазивной хирургии с применением лапароскопических или роботизированных техник, так как такие вмешательства отличаются высоким профилем безопасности и обеспечивают более быстрое восстановление в послеоперационном периоде.
В ходе лечения рака матки 2 стадии, как правило, выполняются более обширные хирургические вмешательства, поскольку несмотря на то, что опухоль все еще локализуется в пределах органа, она распространяется на шейку матки. Для достижения лучших результатов лечения и снижения риска развития рецидива операция может дополняться другими видами терапии, включая лучевую терапию, а также иногда химиотерапию.
Тактика лечения рака матки 3 стадии, на которой происходит распространение опухоли за пределы матки на близлежащие ткани или лимфатические узлы, зачастую предполагает проведение комбинированного лечения, сочетающего хирургическое вмешательство, лучевую терапию и системную химиотерапии. Лучевая терапия используется для контроля локализованного онкопроцесса, а химиотерапия – для предотвращения возможного распространения злокачественной опухоли в отдаленные органы. Каждая схема лечения тщательно разрабатывается с учетом гистологического подтипа новообразования, степени злокачественности опухоли и общего состояния здоровья пациентки.
Благодаря осведомленности о всех возможных вариантах лечения рака матки и соблюдению рекомендаций по терапии рака эндометрия, базирующихся на данных доказательной медицины, у врачей есть возможность составлять для каждой пациентки индивидуальную схему лечения, выбирая наиболее подходящие лечебные процедуры для борьбы с раком эндометрия с учетом стадии заболевания. Такой подход к лечению обеспечивает оптимальные результаты при минимальном профиле побочных эффектов.
Инновационные достижения в лечении рака матки
Хирургические вмешательства, лучевая терапия и химиотерапия по-прежнему составляют основу лечения рака матки. Однако благодаря достижениям современной медицины теперь пациенткам с этим диагнозом также доступны другие высокоэффективные методы лечения, позволяющие значительно улучшить терапевтические результаты и снизить количество побочных эффектов. Особого внимания среди них заслуживают терапия дендритными клетками и гипертермическая интраперитонеальная химиотерапия (HIPEC), продемонстрировавшие успешные результаты в борьбе с раком матки за счет более точного и агрессивного воздействия на онкопроцесс.
Наряду с этими инновационными лечебными процедурами, все более важную роль в борьбе с раком эндометрия приобретают интервенционные процедуры – малоинвазивные, но при этом эффективные вмешательства. Именно за такими инновационными методами лечения будущее лечения рака матки. Они обеспечивают прекрасные результаты, поскольку ориентированы на персонализированный подход к лечению с учетом потребностей каждой пациентки.
Терапия дендритными клетками: активация естественных защитных механизмов иммунной системы
Терапия дендритными клетками – это форма иммунотерапии, при которой для борьбы с раком задействуются естественные защитные механизмы организма. Дендритные клетки являются мощными антигенпрезентирующими клетками: они захватывают и специфическим образом обрабатывают опухолевые антигены, после чего представляют их Т-клеткам, запуская тем самым мощный иммунный ответ, направленный на таргетное уничтожение раковых клеток.
В основе данного терапевтического подхода лежат новаторские научные труды Ральфа М. Штейнмана – первооткрывателя дендритных клеток, который в 2011 году был удостоен Нобелевской премии по физиологии и медицине [4] за установление их важнейшей роли в регуляции работы иммунной системы. Благодаря десятилетиям исследований, проведенных с момента этого революционного открытия, терапия дендритными клетками стала перспективным методом лечения онкологических заболеваний, включая рак матки. Целью этого терапевтического подхода является «обучение» собственной иммунной системы пациента более эффективно распознавать и атаковать раковые клетки, обеспечивая тем самым более целенаправленное и персонализированное лечение с потенциально меньшим количеством побочных эффектов по сравнению с традиционной химиотерапией.
В контексте лечения рака матки терапия дендритными клетками выступает в качестве высокоэффективного и персонализированного подхода, особенно если речь идет о прогрессирующих или рецидивирующих формах заболевания, при которых традиционные виды терапии во многих случаях оказываются малоэффективными. Суть этого инновационного метода состоит в выделении собственных дендритных клеток из крови пациентки, их специальном «программировании» опухоль-специфическими антигенами и повторном введении в организм онкобольной для активации мощного, таргетного противоракового иммунного ответа. Клинические данные уже демонстрируют положительные результаты: терапия дендритными клетками не только способствует более эффективному контролю над опухолью, но и снижает риск развития серьезных побочных эффектов, которые часто сопровождают традиционные методики лечения. Благодаря способности точно активировать естественные защитные механизмы иммунной системы, данный метод лечения рассматривается как революционное решение для пациенток, стремящихся к получению максимально эффективного результата.
HIPEC: высокоэффективная регионарная химиотерапия
Данный передовой метод лечения рака эндометрия предназначен для борьбы с онкопроцессом, распространившимся на брюшную полость, включая поздние стадии рака с метастазами. Процедура HIPEC проводится в два этапа: сначала выполняется хирургическое вмешательство, целью которого является удаление всех видимых опухолей, после чего непосредственно в брюшную полость вводится подогретый до высоких температур раствор химиопрепаратов.
Гипертермическая составляющая метода HIPEC (обычно раствор химиопрепаратов нагревается до 41-43°C) способствует повышению эффективности химиотерапии за счет нескольких механизмов. [5] Нагревание химиопрепаратов помогает увеличить проницаемость мембран раковых клеток, способствуя их более глубокому проникновению в злокачественные ткани, а также провоцирует нарушение механизмом репарации раковых клеток и повышение цитотоксичности некоторых лекарственных средств. Важно отметить, что локальное введение химиотерапевтических препаратов позволяет достичь значительно более высоких их концентраций непосредственно в онкологическом очаге, при этом снижая системное воздействие лечения и связанные с ним побочные эффекты.
Как правило, процедура HIPEC выполняется сразу же после хирургического вмешательства. Её целью является уничтожение всех оставшихся микроскопических раковых клеток, что способствует улучшению общих показателей выживаемости и снижению риска развития рецидива у тщательно отобранных пациентов.
HIPEC обладает доказанной эффективностью и поэтому считается одним из основных вариантов лечения рака эндометрия у пациенток с поздними стадиями заболевания, сопровождающимися поражением органов брюшной полости. Для успешного и безопасного проведения процедуры HIPEC требуется тщательная оценка состояния пациентки. Тем не менее, постоянное совершенствование метода способствует расширению доступа к лечению и повышению его эффективности.
Представляем вашему вниманию эксклюзивное интервью с доктором Липпом – одним из ведущих специалистов Германии в области лечения методом HIPEC. В беседе доктор Липп рассказывает о впечатляющих возможностях этой процедуры в лечении рака, особенностях её проведения и результатах лечения.
Ведущий немецкий хирург доктор Липп о преимуществах метода HIPEC
Методы интервенционной радиологии в борьбе с раком матки
Инновационные интервенционные вмешательства обеспечивают органосохраняющее лечение рака эндометрия, особенно при прогрессирующих, рецидивирующих или неоперабельных формах заболевания. Эти малоинвазивные процедуры выполняются под визуальным контролем и позволяют воздействовать непосредственно на опухоль, не затрагивая при этом окружающие здоровые ткани. Такое лечение имеет особо важное значение для пациенток с раком матки, которым противопоказана полноценная хирургическая операция или которым требуется комбинированное лечение с применением локальных процедур и системной терапии.
В настоящее время в клинической практике успешно применяется весь спектр представленных ниже интервенционных методов лечения рака матки и его метастазов.
Таргетное уничтожение опухоли с помощью инновационных регионарных форм химиотерапии TACE и TACP
Трансартериальная химиоэмболизация (TACE), также известная как химиоабляция, – это малоинвазивная процедура, которая всё чаще применяется в современном лечении рака матки (эндометрия), особенно у пациенток с метастатическими поражениями в области малого таза, резистентными к системной терапии. Изначально процедура TACE была разработана для лечения опухолей печени, однако впоследствии она продемонстрировала многообещающие результаты и в области гинекологической онкологии, в том числе при лечении прогрессирующего или рецидивирующего рака матки с метастатическими поражениями тазовой области, лимфатических узлов или печени.
Процедура TACE проводится в два этапа. На первом этапе интервенционный радиолог через бедренную или лучевую артерию вводит микрокатетер, который под визуальным контролем продвигается к кровеносным сосудам, питающим опухоль. После его установки в таргетной зоне непосредственно в артерию, обеспечивающую кровоснабжение опухоли, вводится высококонцентрированная доза химиотерапевтических препаратов. На втором этапе процедуры в просвет этой же артерии вводятся эмболизирующие вещества, которые блокируют приток крови к опухоли, одновременно обеспечивая эффективное удержание лекарственных средств в микроокружении опухоли. Таким образом, техника TACE обеспечивает мощное локализованное воздействие на онкологический очаг химиопрепаратами, а также одномоментно лишает опухоль кислорода и питательных веществ, что приводит к ее некрозу.
Трансартериальная химиоперфузия (TACP) – техника, схожая по принципу действия с TACE, но со своими отличительными особенностями, которая рассматривается как дополнительный вариант лечения рака. В отличие от TACE, процедура TACP не предусматривает выполнение эмболизации сосудов, питающих злокачественную опухоль. Напротив, ее суть заключается в высокопоточном введении химиопрепаратов непосредственно в сосудистую сеть, обеспечивающую приток крови к опухоли, но без последующей блокировки просвета питающих артерий. Техника TACP обеспечивает значительно лучшее проникновение цитостатиков в опухоли с диффузным или инфильтративным типом васкуляризации, характерного для поздних стадий рака матки, которые сопровождаются поражением органов малого таза.
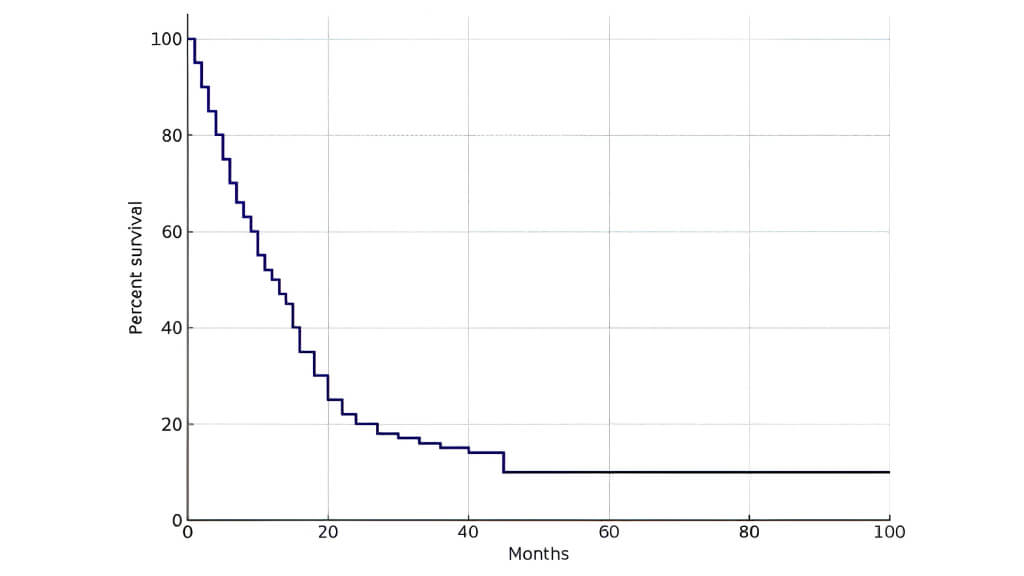
Результаты последних исследований также подтверждают клиническую эффективность этих методов: сравнительный анализ продемонстрировал, что такое лечение приводит к статистически значимому уменьшению размера опухоли. При оценке эффективности TACE и TACP по стандартизированным критериям ответа на лечение обе процедуры показали благоприятное распределение полных и частичных ответов на терапию. Кроме того, по результатам анализа показателей выживаемости среди всей когорты пациенток, получивших такое лечение, медиана общей выживаемости составила 16,15 месяцев. Эти данные свидетельствует о том, что процедуры TACE и TACP обладают потенциалом оказывать существенное влияние на контроль над заболеванием и улучшать результаты лечения пациенток с поздними стадиями рака. [6]
| Группа пациенток | Количество пациенток | Средний объем опухоли в начале исследования (см³) | 3-месячное наблюдение | 6-месячное наблюдение | 9-месячное наблюдение |
|---|---|---|---|---|---|
| Группа 1 | 46 | 117 | 98.48 | - | - |
| Группа 2 | 19 | 117.27 | 77.99 | 68.78 | - |
| Группа 3 | 10 | 103.4 | 86 | 80.87 | 119.71 |
*Ответ на терапию и показатели выживаемости пациенток с гинекологическими опухолями, прошедших лечение методами трансартериальной химиоперфузии и трансартериальной химиоэмболизации [6]
Оценка ответа опухоли на лечение при применении различных терапевтических протоколов
| Ответ опухоли на лечение | TACP (количество, %) | TACE (количество, %) | TACP + TACE (количество, %) |
|---|---|---|---|
| Стабилизация заболевания | 23 (70) | 10 (50) | 18 (82) |
| Частичный ответ на лечение | 6 (18) | 3 (15) | - |
| Полный ответ на лечение | 1 (3) | 1 (5) | - |
| Прогрессирование заболевания | 3 (9) | 6 (30) | 4 (18) |
| Пациентки, у которых наблюдался ответ на терапию | 30 (91) | 14 (70) | 18 (82) |
*Ответ на терапию и показатели выживаемости пациенток с гинекологическими опухолями, прошедших лечение методами трансартериальной химиоперфузии и трансартериальной химиоэмболизации [6]
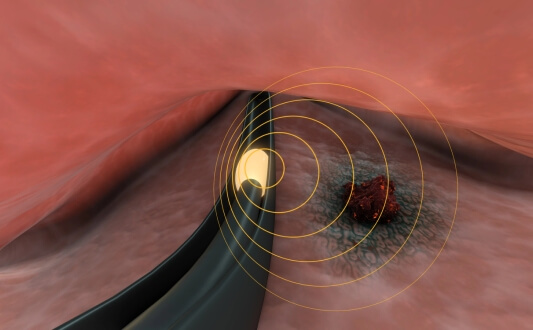
Радиоабляция (радиочастотная абляция)
Радиочастотная абляция (РЧА) – метод, при котором для разрушения злокачественной ткани используется тепловая энергия. Под визуальным контролем непосредственно в опухоль вводится специальный игольчатый электрод, через который проходит высокочастотный электрический ток. В результате генерируется тепло, вызывающее некроз опухоли.
У пациенток с раком матки РЧА может применяться для лечения локальных рецидивов рака или метастатических поражений малого таза, лимфатических узлов, легких, печени. Радиочастотная абляция является высокоточным методом лечения, что позволяет свести к минимуму риск повреждения близлежащих органов. Метод имеет особую ценность для пациенток, которым противопоказана хирургическая операция или лучевая терапия. РЧА характеризуется минимальным дискомфортом и часто проводится амбулаторно.
Данная процедура помогает уменьшить опухолевую нагрузку, облегчить болевой синдром и замедлить прогрессирование заболевания, способствуя улучшению общего качества жизни онкобольной.
Лечение рака матки криоаблацией
Криоабляция – метод, в основе которого лежит воздействие на раковые клетки экстремально низкими температурами с целью их уничтожения. Процедура проводится под визуальным контролем. Непосредственно в опухоль вводится зонд, из которого подается замораживающий газ, формируя «ледяной шар». В результате происходит разрушение клеточных структур и блокируется кровоснабжение новообразования.
Этот метод обладает высокой эффективностью в лечении метастатического или рецидивирующего рака матки с локализацией в мягких тканях, лимфатических узлах или костях. К преимуществам метода относятся четкая визуализация в ходе терапевтической процедуры и возможность подбора зонда в точном соответствии с размером и локализацией опухоли.
Как правило, криоабляция проводится под местной анестезией и вызывает минимальное повреждение тканей за пределами таргетной зоны. Криоабляция обеспечивает превосходный контроль над симптомами рака. Восстановление после процедуры происходит предельно быстро. При необходимости есть возможность повторного проведения лечебной манипуляции.
Термоабляция (микроволновая абляция)
Микроволновая абляция (МВА) – один из видов термоабляции, основанный на использовании электромагнитной энергии для генерации тепла, которое впоследствии разрушает опухолевую ткань. По сравнению с РЧА, МВА способна генерировать более высокие температуры, что позволяет проводить лечение опухолей более крупного размера с более эффективными результатами.
При лечении рака эндометрия возможность проведения МВА рассматривается при метастатических поражениях печени или легких, а также для исключения развития рецидива в области малого таза. Микроволновая абляция также применяется в случаях, когда хирургическое вмешательство невозможно или пациентка не в состоянии перенести слишком инвазивную операцию.
МВА – это быстрый, точный и безопасный метод лечения, обеспечивающий превосходный локальный контроль над опухолью при минимальном воздействии техники на здоровые ткани. Данную процедуру довольно часто проводят в рамках комплексного лечения в сочетании с системной терапией.
| Вид терапии | Показатели 2-летней выживаемости | Вид терапии | Продолжительность курса лечения | Побочные эффекты |
|---|---|---|---|---|
| Стандартные методы лечения | ~55-70% на ранних стадиях рака ~30% на поздних стадиях рака | Менее 10% | От нескольких недель до нескольких месяцев | Умеренные и тяжелые побочные эффекты (повышенная утомляемость, тошнота, бесплодие, нарушения в работе кишечника/мочевого пузыря) |
| Инновационные методы лечения | ~60-75% в отдельных случаях при прогрессирующем/рефрактерном раке | 45-65% | До 4-6 сеансов | Незначительные побочные эффекты (лихорадка, локализованный воспалительный процесс, гриппоподобные симптомы) |
*Таблица составлена на основе клинических данных Booking Health и опубликованных результатов исследований. Фактические результаты лечения могут отличаться в зависимости от состояния пациентки и применяемого протокола лечения.
История Сюзанны и ее успешный опыт лечения прогрессирующего рака матки за границей с Booking Health
Когда у Сюзанны Линн О’Донохью из Великобритании диагностировали рак эндометрия на поздней стадии, она решила не терять времени и приступила к поиску эффективного лечения за пределами родной страны. В результате у женщины возникло множество вопросов, ответы на которые найти было непросто. Столкнувшись с трудностями в организации поездки на лечение за рубеж, Сюзанна обратилась в компанию Booking Health. Именно это решение стало поворотным моментом. Профессиональная помощь этого авторитетного оператора медицинского туризма привнесла ясность в процесс, а также обеспечила такую необходимую Сюзанне поддержку. Благодаря сотдуничнству с Booking Health пациентка своевременно получила доступ к обслуживанию в одной из ведущих клиник Германии, специализирующихся на лечении рака матки.
Специалисты компании Booking Health организовали для Сюзанны программу лечения во Франкфурте, благодаря чему она смогла получить квалифицированную помощь врачей с экспертным опытом в области лечения рака эндометрия (матки) в престижной клинике. С первого же контакта с сотрудниками Booking Health Сюзанна ощутила их поддержку. Они с пониманием отнеслись не только к её сложному диагнозу, но и к глубокому эмоциональному потрясению, которое ей пришлось испытать. Решением всех логистических вопросов – от организации приемов в клинике до перевода в ходе консультаций с врачами – занимались сотрудники Booking Health. С поставленными задачами они справились на отлично.
Ключевой фигурой в истории Сюзанны стала Афсане – её личный медицинский координатор. «Благодаря ей все прошло максимально гладко. Она оказывала помощь по всем вопросам, благодаря чему лечение было максимально успешным, и при этом в ходе всего процесса не было никаких трудностей», – вспоминает Сюзанна. Многие врачи свободно говорили по-английски, но именно благодаря профессиональному переводу Афсане Сюзанна и её семья четко понимали каждый медицинский термин, особенности каждого этапа лечения рака матки и каждый аспект терапевтического процесса.
Благодаря профессиональной помощи компании Booking Health в организации лечения в Германии и самоотверженной поддержке Афсане, Сюзанна смогла сосредоточиться на самом важном – на своем выздоровлении. Её история является ярким примером того, как при поддержке надежного партнера лечение рака за рубежом может стать не сложным испытанием, а успешным опытом, способным подарить надежду на будущее.
Будь то лечение рака матки или другой сложный диагноз, опыт таких пациенток, как Сюзанна, наглядно демонстрирует, что сотрудничество с профессиональным оператором медицинского туризма дает возможность не просто получить доступ к передовой медицинской помощи за рубежом, но и кардинально изменить свою жизнь.

Даже на поздней стадии рака всегда есть шанс на жизнь
Пациентки с диагнозом «рак матки на поздней стадии» или «рецидив рака эндометрия» зачастую сталкиваются с сильным эмоциональным потрясением, при этом им приходится принимать сложные решения. Женщин с поздними стадиями заболевания, в том числе тех, которым необходимо лечение рака матки 4 стадии, беспокоят прогнозы, потенциальный риск развития рецидива онкопатологии и ограниченные возможности лечения. Однако стоит понимать, что современная медицина развивается стремительными темпами, и сейчас в арсенале врачей есть инновационные разработки, которые способны помочь даже на поздних стадиях рака.
Booking Health – надежный оператор медицинского туризма, который предоставляет доступ к обслуживанию в ведущих европейских онкологических центрах, специализирующихся на проведении наиболее эффективного лечения рака матки, в том числе редких и сложных случаев этого заболевания. В зависимости от конкретной клинической ситуации, лечение может включать хирургическое вмешательство, химиотерапию, гормональную терапию, иммунотерапию или такие инновационные подходы, как интервенционные вмешательства под визуальным контролем. Все эти методики сочетаются в рамках индивидуально составленной для пациентки схемы лечения, направленной на достижение наилучшего результата.
Каждый клинический случай тщательно анализируется, ведь врачам важно разработать для пациентки индивидуальную программу лечения с учетом ее состояния здоровья, ранее проведенного курса терапии и особенностей выявленной у нее опухоли. Такой уровень персонализации критически важен на поздних стадиях рака, когда стандартные подходы часто оказываются неэффективными.
Booking Health гарантирует профессиональную координацию на каждом этапе поездки на лечение за границу – от выбора подходящей клиники и команды врачей до надлежащей подготовки медицинской документации, предоставления услуг устного перевода и организации размещения пациентки в гостинице или апартаментах на период лечения в другой стране. Благодаря комплексной координации у пациенток есть возможность полностью сосредоточиться на восстановлении своего здоровья, в то время как о решении сложных вопросов, связанных с международной логистикой, позаботятся специалисты Booking Health.
Booking Health предоставляет женщинам с прогрессирующим раком матки доступ к передовым методам лечения за границей. Специалисты компании соблюдают в своей работе четкие и структурированные алгоритмы, обеспечивающие высочайшее качество медицинского обслуживания, заботливый уход и ориентацию на индивидуальные потребности пациентки.
Поездка на лечение за границу с Booking Health
Самостоятельный поиск наилучшей тактики лечения с учетом вашей индивидуальной клинической ситуации – это довольно сложная задача. Испытав на себе многочисленные курсы лечения, проконсультировавшись со множеством специалистов и испробовав различные терапевтические процедуры, вам может быть трудно сориентироваться во всей предоставленной врачами информации. В таком случае пациенты зачастую выбирают первый же предложенный вариант лечения или соглашаются на лечение с применением стандартизированных терапевтических протоколов, которое влечет за собой множество побочных эффектов, вместо того, чтобы рассмотреть возможность терапии с помощью инновационных процедур.
Если вы хотите сделать осознанный выбор и получить лечение рака в соответствии с индивидуально разработанной для вас схемой с учетом особенностей вашей конкретной клинической ситуации, проконсультируйтесь с врачами-консультантами Booking Health. Компания Booking Health уже более 12 лет занимает ведущие позиции в сфере организации лечения за рубежом с применением новейших инноваций в медицине, поэтому ее специалисты обладают огромным опытом в составлении персонализированных комплексных программ лечения для каждого пациента. Booking Health пользуется репутацией авторитетной компании, которая предоставляет персонализированный подбор схемы лечения рака матки и клиники с прямым бронированием приема в медицинском центре и полной поддержкой на каждом этапе лечения – от решения организационных вопросов до помощи в процессе лечения. Мы предлагаем:
- Оценку и анализ медицинских заключений пациентки
- Составление индивидуальной программы лечения
- Подбор подходящего медицинского учреждения для лечения
- Подготовку медицинской документации и ее направление в выбранную пациенткой для лечения клинику
- Консультации с врачами зарубежной клиники для разработки оптимальной медицинской программы на этапе подготовки к поездке на лечение
- Экспертные консультации во время пребывания в больнице
- Последующее консультирование пациентки после ее возвращения на родину по завершении медицинской программы
- Решение организационных вопросов в рамках подготовки к поездке на лечение за границу
- Координацию и организацию пребывания пациентки в другой стране, помощь в бронировании номера в отеле или апартаментов на период лечения
- Помощь в оформлении визы и бронировании авиабилетов
- Услуги переводчика и персонального координатора, который будет с вами на связи 24/7
- Прозрачные цены на лечение без скрытых платежей
Здоровье – главная ценность в жизни каждого человека, доверять заботу о которой стоит лишь лучшим специалистам с богатым опытом и проверенной репутацией. Booking Health – это ваш надежный партнер, который оказывает всестороннюю помощь на пути к восстановлению здоровья и улучшению качества жизни. Свяжитесь с врачом-консультантом компании, чтобы узнать больше о возможностях персонализированного лечения рака матки у ведущих экспертов с использованием инновационных методов.
Инновации в онкологии: опыт пациентов Booking Health
Частые вопросы о раке матки (эндометрия) и его лечении
Отправить запрос на лечениеВыбор наиболее эффективного метода лечения зависит от стадии рака, конкретного типа опухоли и общего состояния здоровья женщины. Для лечения карцином на ранних стадиях во многих случаях выполняются хирургические вмешательства (в основном гистерэктомия). На поздних стадиях заболевания зачастую требуется комплексное лечение с включением в схему химиотерапии, лучевой терапии или иммунотерапии.
Как правило, на первом этапе диагностического обследования в гинекологии проводится проверка на наличие кровотечений и осмотр органов малого таза, а также выполняются визуализационные исследования. Для подтверждения наличия злокачественного процесса проводится биопсия слизистой оболочки матки. Что касается алгоритмов определения стадии рака эндометрия, для этого требуется выполнение визуализационных исследований, позволяющих подтвердить или исключить наличие метастазов. На основании результатов этих исследований онкологи составляют оптимальную для пациентки схему лечения.
Схема лечения может включать хирургическое вмешательство (в том числе роботизированные или лапароскопические операции), лучевую терапию, химиотерапию, гормональную терапию, иммунотерапию. Каждый клинический случай рассматривается в рамках междисциплинарного онкологического консилиума, после чего врачи разрабатывают индивидуальную терапевтическую схему с учетом типа и стадии опухоли.
Хирургическое вмешательство (гистерэктомия) является основным методом лечения большинства случаев рака эндометрия. Однако, если операция невозможна из-за сопутствующих проблем со здоровьем или желания женщины сохранить репродуктивную функцию, возможно применение нехирургических методов лечения, например, гормональной терапии или лучевой терапии.
Гистерэктомия – это операция по удалению матки. При раке матки данное вмешательство во многих случаях является методом лечения первой линии, особенно на ранних стадиях заболевания. Гистерэктомия проводится с помощью лапароскопических или роботизированных техник, иногда также предполагает удаление шейки матки и яичников.
Да, в некоторых случаях на ранних стадиях рака эндометрия, особенно у пациенток молодого возраста, желающих сохранить репродуктивную функцию, вместо операции применяется гормональная терапия. Однако долгосрочный успех такого лечения зависит от динамики роста опухоли. В таких ситуациях требуется пристальное наблюдение онколога.
Химиотерапия вызывает повышенную утомляемость, тошноту, выпадение волос, снижение уровня эритроцитов, лейкоцитов и тромбоцитов в крови, повышенный риск развития инфекции. Цитостатики уничтожают раковые клетки, в том числе за пределами матки. Химиотерапия может применяться после операции для снижения риска развития рецидива.
При облучении для уничтожения злокачественных клеток в матке, малом тазе или близлежащих лимфатических узлах используется высокоэнергетическое излучение. Лучевая терапия может применяться после операции или в тех случаях, когда нет возможности удалить опухоль хирургическим путем. В зависимости от стадии рака матки проводится внешняя лучевая терапия или внутреннее облучение (брахитерапия).
Риск развития рецидива зависит от степени злокачественности опухоли, стадии заболевания и проведенного лечения. Решающую роль в предотвращении рецидива рака эндометрия играют регулярные скрининги и последующее наблюдение. При некоторых типах рака высокого риска, например, папиллярной или серозной карциноме, может потребоваться применение более агрессивной тактики лечения с целью улучшения прогноза пациентки.
Да, иммунотерапия является перспективным методом лечения рака матки, особенно при прогрессирующих или рецидивирующих формах заболевания с определенными генетическими маркерами. Она помогает иммунной системе лучше распознавать и атаковать раковые клетки и довольно часто включается в современные схемы лечения онкологических заболеваний.
В некоторых случаях у женщины есть возможность забеременеть после консервативного лечения рака эндометрия на ранних стадиях гормональной терапией. Однако стандартные подход к лечению обычно предполагает проведение гистерэктомии – операции по удалению матки, что приводит к потере естественной фертильности. Решение о возможности проведения лечения рака матки, которое позволило бы сохранить репродуктивную функцию при раке матки должно приниматься онкологом.
К числу новых методов лечения рака эндометрия относятся терапия дендритными клетками, HIPEC (гипертермическая интраперитонеальная химиотерапия) и TACE (трансартериальная химиоэмболизация). Эти методики направлены на снижение частоты рецидивов и улучшение показателей выживаемости.
Гормональная терапия применяется при гормоночувствительных формах рака эндометрия, особенно на ранних стадиях или у пациенток, желающих сохранить фертильность. Такое лечение помогает замедлить рост опухоли, воздействуя на клетки слизистой оболочки матки. Гормональная терапия может применяться в качестве самостоятельного метода или в сочетании с другими видами лечения рака.
Стоимость лечения рака матки варьируется в зависимости от страны, в которой оно будет проходить, назначенной пациентке терапевтической схемы, уровня клиники и необходимых методов лечения, в частности хирургическое вмешательство, химиотерапия или лучевая терапия. Booking Health помогает иностранным пациентам найти экономически выгодные варианты высококачественного лечения рака, включая обеспечение услуги «второе мнение» и полной координации поездки за границу.
Выбирайте лечение за рубежом и Вы, несомненно, получите отличный результат!
Авторы:
Статья составлена под редакцией экспертов в области медицины, врачей-специалистов доктора Надежды Иванисовой и доктора Богдана Михальнюка. Для лечения состояний, о которых идет речь в статье, необходимо обратиться к врачу; информация в статье не предназначена для самолечения!
С редакционной политикой, которая отражает наше стремление к точности и прозрачности, можно ознакомиться здесь. Перейдите по ссылке, чтобы ознакомиться с нашими правилами.
Источники:
[1] European Cancer Information System (ECIS). Cancer burden in EU-27 countries. 2022. https://ecis.jrc.ec.europa.eu
[2] European Network of Cancer Registries (ENCR). https://encr.eu
[3] European Society for Medical Oncology (ESMO). Endometrial cancer: ESMO Clinical Practice Guidelines. https://www.annalsofoncology.org/article/S0923-7534(22)01207-8/fulltext
[4] The Nobel Prize. The Nobel Prize in Physiology or Medicine 2011 – Ralph M. Steinman. https://www.nobelprize.org/prizes/medicine/2011/steinman/facts
[5] MDPI. The Role of Hyperthermic Intraperitoneal Chemotherapy in Uterine Cancer Therapy. https://www.mdpi.com/1422-0067/24/15/12353
[6] MDPI. Therapy Response and Survival among Patients with Gynecologic Tumors Treated with Transarterial Chemoperfusion and Transarterial Chemoembolization. https://www.mdpi.com/1648-9144/60/10/1585
Читайте:
Меню статьи:
- Общая информация о раке эндометрия
- Стандартные подходы к лечению рака эндометрия
- Инновационные достижения в лечении рака матки
- Методы интервенционной радиологии в борьбе с раком матки
- История Сюзанны и ее успешный опыт лечения прогрессирующего рака матки за границей с Booking Health
- Даже на поздней стадии рака всегда есть шанс на жизнь
- Поездка на лечение за границу с Booking Health
- Частые вопросы о раке матки (эндометрия) и его лечении
Не знаете, с чего начать?
Свяжитесь с Booking Health