Рак тела матки (эндометрия) 4 стадии – это наиболее тяжелая стадия карциномы эндометрия, при которой рак распространяется за пределы матки на отдаленные органы: легкие, печень, кости или лимфатические узлы. По данным Американского онкологического общества, рак матки является наиболее распространенным гинекологическим злокачественным заболеванием. Ежегодно только в США регистрируется более 66 000 новых случаев этой онкопатологии.
Примерно в 10-15% случаев рак матки диагностируется на 4 стадии. На этом этапе развития заболевания оно становится метастатическим, что существенно усложняет процесс лечения и ухудшает прогноз. Пятилетняя выживаемость при раке эндометрия 4 стадии варьируется в пределах 15-20% в зависимости от общего состояния пациентки, проведенного курса лечения и степени распространения онкопроцесса.
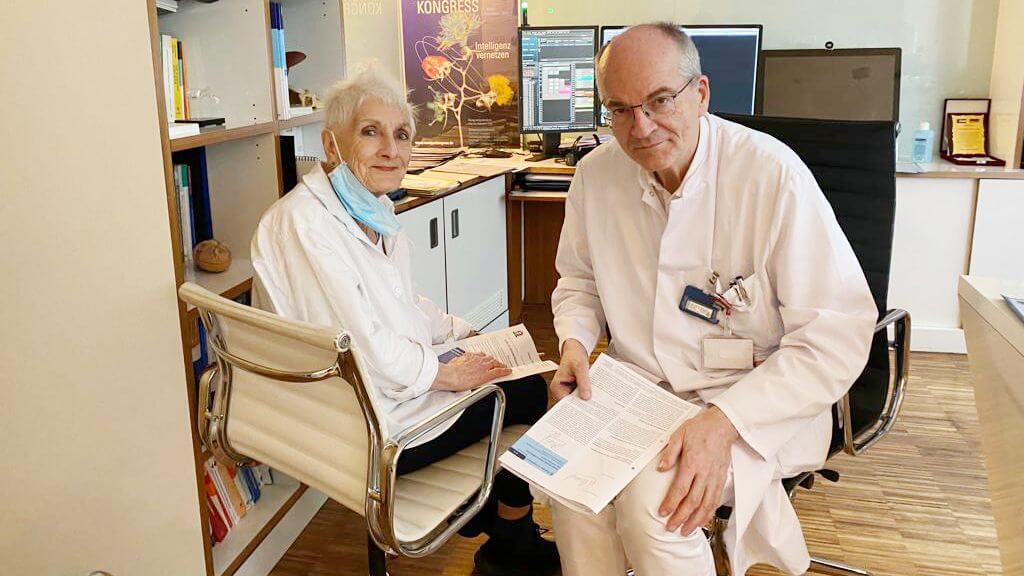
Решающую роль в успешности лечения пациенток с этим сложным диагнозом играет квалифицированная помощь онкогинекологов и персонализированный подход к терапии. Ведущие специалисты с богатым опытом составляют для каждой пациентки индивидуальную схему лечения с интеграцией в нее инновационных методик, благодаря чему даже в самых сложных клинических ситуациях у женщины есть шанс на хороший результат.
Стандартные протоколы лечения
При лечении рака тела матки 4 стадии обычно используется мультимодальный подход – в схему лечения включается несколько видов терапии. Все они направлены на достижение контроля над заболеванием и облегчение симптомов.
Хирургическое лечение применяется лишь в отдельных случаях, предполагает выполнение гистерэктомии (операции по удалению матки) и лимфодиссекции. Ввиду обширного распространения онкопроцесса на 4 стадии операция сама по себе редко выступает в качестве куративного (излечивающего) варианта лечения. Как правило, хирургическое вмешательство является лишь частью комплексной схемы лечения рака матки 4 стадии.
Лучевая терапия используется для контроля роста опухоли и облегчения симптомов рака эндометрия 4 стадии, включая боли в области таза и маточные кровотечения. Облучение помогает уменьшить размеры опухоли и улучшить самочувствие пациентки, особенно в тех случаях, когда ей противопоказано проведение хирургического вмешательства.
Химиотерапия является основным методом системного лечения рака эндометрия 4 стадии. Она помогает замедлить прогрессирование онкозаболевания, но при этом вызывает серьезные побочные эффекты: повышенную утомляемость, тошноту, выпадение волос, подавление иммунитета.
Гормональная терапия проводится при гормон-рецептор-положительном раке матки. В ходе лечения применяются прогестины, ингибиторы ароматазы или селективные модуляторы рецепторов эстрогена (СМРЭ), препятствующие росту опухоли, обусловленного синтезом гормонов. Этот вариант лечения обычно менее агрессивен и подходит пациенткам с противопоказаниями к химиотерапии.
Паллиативная помощь играет важнейшую роль в лечении рака эндометрия поздней стадии. Она направлена на облегчение болевого синдрома, стабилизацию психоэмоционального состояния пациентки и повышение качества ее жизни. Паллиативная помощь используется в комплексе с другими видами терапии или в качестве самостоятельного метода лечения последней стадии онкозаболевания.
Рак матки 4 стадии – это агрессивное заболевание, зачастую резистентное к традиционным методам лечения, поэтому стандартная терапия далеко не всегда помогает продлить жизнь пациентки с этой онкопатологией. Это послужило стимулом к исследованию и внедрению в клиническую практику новых таргетных методов лечения, которые могли бы улучшить результаты и обеспечить более широкий спектр возможностей терапии для пациенток с раком матки 4 стадии, которым не помогает лечение по стандартному протоколу.
Инновационные методы лечения
По мере развития направления онкологии появляются новые лечебные процедуры, которые позволяют улучшить показатели выживаемости пациенток с раком матки 4 стадии. Эти инновационные методики обеспечивают более эффективный результат при рецидивах опухоли, метастатическом раке и резистентности заболевания к химиотерапии, что в свою очередь способствует улучшению долгосрочных результатов и повышению качества жизни пациентки.
Интервенционная радиология
Одним из фокусов работы направления интервенционной радиологии является проведение передовых малоинвазивных процедур для лечения рака матки. Они выступают в качестве особо ценной альтернативы при рецидиве этой онкопатологии и при невозможности проведения традиционного лечения. Интервенционные вмешательства выполняются под визуальным контролем, за счет чего обеспечивается высокоточное прицельное воздействие на опухолевый очаг при минимальном повреждении здоровых тканей. Такое лечение проводится женщинам с распространенным или метастатическим раком матки как в паллиативных целях для облегчения симптомов, так и для достижения контроля над заболеванием. При этом по сравнению с традиционными видами терапии восстановление после интервенционных процедур обычно происходит гораздо быстрее, практически отсутствуют системные побочные эффекты.
Термоабляция – один из наиболее широко распространенных методов абляции, при котором коагуляционный некроз в опухолевых тканях обеспечивается за счет воздействия на них высокими температурами. Первоначально метод предназначался для лечения опухолей печени и легких, но в последнее время его также начали применять в сфере онкогинекологии, в частности при лечении рецидивирующих или неоперабельных злокачественных опухолей матки. По результатам исследований, проведение термоабляции в комбинации с системной химиотерапией или облучением в более 78% случаев позволяет добиться локального контроля над онкопроцессом на период 12 месяцев, особенно у пациенток с локализованными рецидивами рака эндометрия в области таза. Следовательно, термоабляция расценивается в качестве щадящего терапевтического метода, который обычно интегрируется в комплексную схему лечения.
Криоабляция – эффективный метод деструкции опухоли при помощи экстремально низких температур, обладающий рядом преимуществ по сравнению со стандартными вариантами лечения злокачественных новообразований. Криоабляция чаще всего используется в лечении рака почек и предстательной железы, но сейчас эту процедуру также проводят при рецидивирующем раке эндометрия, в том числе при невозможности выполнения хирургического вмешательства.
Исследования продемонстрировали, что в 80% случаев проведение криоабляции позволяет обеспечить беспрогрессивную выживаемость на период 6 месяцев. При этом процедура хорошо переносится пациентками и практически не оказывает негативного воздействия на здоровые соседние ткани. Криоабляция относится к щадящим видам терапии, которые могут использоваться в качестве паллиативного лечения при необходимости проведения повторной операции или при метастатических поражениях вблизи жизненно важных анатомических структур.
Электрохимиотерапия (ЭХТ) – лечебная процедура, при которой воздействие на онкологический очаг короткими электрическими импульсами сочетается с одномоментным локальным введением химиопрепаратов, за счет чего удается добиться лучшего терапевтического эффекта. Этот метод чаще всего применяется при метастазах в кожу и стенки таза, но недавно были проведены исследования по оценке эффективности этой процедуры при рецидивирующем раке матки, и полученные результаты весьма обнадеживающие.
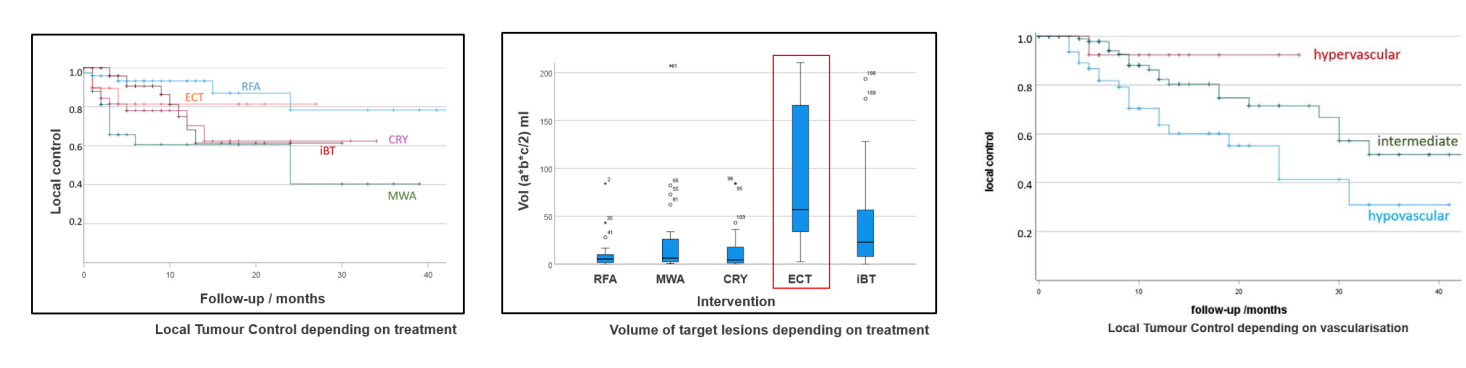
Согласно данным текущих клинических исследований, частота ответа опухоли на ЭХТ составляет более 70%, особенно при использовании метода для лечения поверхностных метастатических поражений органов малого таза. ЭХТ не только обеспечивает прямое цитотоксическое воздействие на онкологический очаг, но также способствует активации иммуноопосредованного ответа опухоли, что свидетельствует о синергетическом эффекте ЭХТ при ее сочетании с иммунотерапией на поздних стадиях заболевания.
Химиоэмболизация (TACE)
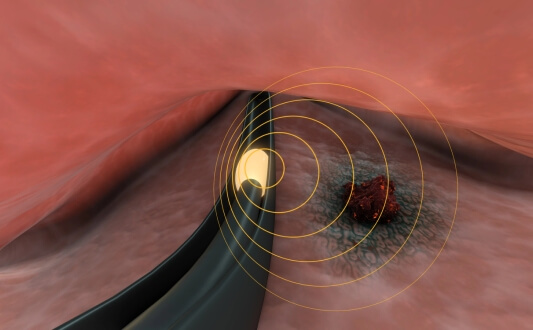
Трансартериальная химиоэмболизация (TACE) – малоинвазивный метод лечения, предполагающий доставку высококонцентрированных доз химиопрепаратов непосредственно к опухоли с одномоментным блокированием ее кровоснабжения. Процедура помогает лишить опухоль кислорода и питательных веществ, а также существенно усилить действие лекарственных препаратов.
Лечение методом TACE отличается особой эффективностью у пациенток с метастатическим раком матки, которым противопоказано хирургическое вмешательство. Процедура дает возможность уменьшить размеры опухоли и замедлить прогрессирование заболевания при меньшем количестве системных побочных эффектов по сравнению с традиционной химиотерапией. Клинические исследования показали, что TACE улучшает ответ опухоли на лечение и повышает показатели продолжительности жизни на последней стадии карциномы эндометрия.
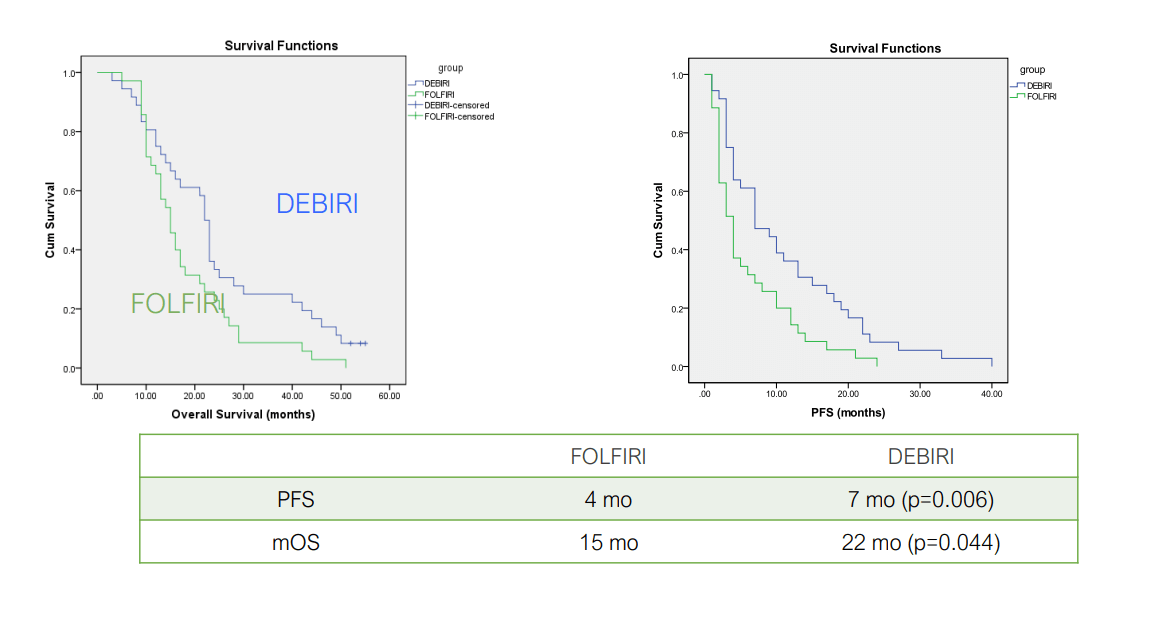
Aliberti C et al Ancancer Res 2011;31:4581
Richardson A et al J Vasc Interv Radiol 2013;24:1209
**DEBIRI = TACE, FOLFIRI = IV therapy
Представляем вашему вниманию эксклюзивное интервью с профессором Томасом Фоглем – ведущим экспертом в сфере интервенционной радиологии и онкологии. В своем интервью специалист рассказывает о принципе действия TACE и ее эффективности в лечении рака на поздних стадиях, а также делится реальными историями успешного лечения пациентов, которые свидетельствуют о преимуществах этого инновационного метода.
Профессор Томас Фогль: как химиоэмболизация меняет подход к лечению рака
Терапия дендритными клетками
Терапия дендритными клетками – это один из видов иммунотерапии, открытие которого было отмечено Нобелевской премией. Основу данного инновационного метода лечения составляет применение специализированных иммунных клеток (дендритных клеток) для повышения способности собственного организма пациента распознавать и атаковать раковые клетки: дендритные клетки извлекают из крови пациента, их «обучают» распознавать опухоль-специфические антигены и повторно вводят в организм пациента для запуска таргетного иммунного ответа, нацеленного на метастатические новообразования.
Методика демонстрирует особенно многообещающие результаты при лечении рака матки 4 стадии, когда традиционные виды терапии часто оказываются неэффективными. По сравнению с химиотерапией лечение дендритными клетками обладает низкой токсичностью, поэтому представляет собой эффективный альтернативный вариант для пациентов, которые не в состоянии перенести лечение рака по стандартному протоколу. По данным исследований, вакцинация дендритными клетками улучшает показатели выживаемости и способствует снижению частоты рецидивов онкологии.
Профессор Франк Гансауге – ведущий специалист в сфере иммунотерапевтического лечения. В своем интервью доктор рассказывает об особенностях проведения терапии дендритными клетками и их роли в качестве «офицеров» иммунной системы, а также делится реальными историями пациентов, которым это инновационное лечение помогло добиться длительной ремиссии.
Профессор Ганcауге раскрывает секреты лечения рака дендритными клетками: от науки к практике
HIPEC (гипертермическая интраперитонеальная химиотерапия)
Гипертермическая интраперитонеальная химиотерапия (HIPEC) – это инновационный метод лечения, предназначенный для пациентов с метастатическим поражением брюшной полости, в том числе при раке эндометрия 4 стадии. Суть процедуры заключается в хирургическом удалении видимых опухолей из брюшной полости с последующим ее промыванием раствором подогретых до высоких температур химиопрепаратов для уничтожения оставшихся раковых клеток. Нагревание раствора химиопрепаратов повышает их эффективность, благодаря чему по сравнению со стандартными внутривенными методами введения лекарственных средств обеспечивается их лучшее проникновение в раковые клетки и лучший эффект лечения. HIPEC продемонстрировала многообещающие результаты при прогрессирующем раке женских половых органов: при применении этого метода лечения отмечается повышение показателей выживаемости и снижение частоты рецидивов. Одним из ключевых преимуществ HIPEC является ее способность доставлять высокую дозу химиопрепаратов к онкологическому очагу, минимизируя при этом системные побочные эффекты.
Доктор Михаэль Липп – заведующий отделением абдоминальной и колоректальной хирургии Клиники Асклепиос Бармбек Гамбург. В своем эксклюзивном интервью доктор Липп рассказывает об особенностях проведения процедуры HIPEC и критериях отбора пациентов, а также делится реальными историями пациентов, подтверждающими высокую эффективность метода.
Ведущий немецкий хирург доктор Липп о преимуществах HIPEC в лечении рака
Гипертермия
В отличие от HIPEC гипертермия является неинвазивным или малоинвазивным методом лечения, при котором терапевтический эффект достигается за счет воздействия на опухолевые ткани высокими температурами (обычно 40-43°C). Эта процедура применяется для повышения эффективности традиционных видов терапии рака. Гипертермия обладает способностью повышать чувствительность раковых клеток к химиопрепаратам и облучению, нарушать механизмы их восстановления, усиливать кровоток для лучшей доставки лекарств к опухолевому очагу и стимулировать иммунную активность, поэтому в контексте лечения рака матки 4 стадии она используется в качестве дополнения к химиотерапии и лучевой терапии. Исследования показали, что проведение гипертермии в комбинации с лучевой терапией позволяет уменьшить размер опухоли и добиться локального контроля онкопроцесса на поздних стадиях гинекологического рака, включая рак эндометрия.
Радиочастотная и микроволновая гипертермия считаются наиболее прогрессивными видами этого метода лечения. Они дают возможность прицельно воздействовать на опухоли и метастатические поражения в области малого таза, используя регионарную технику или гипертермию всего тела. Первые полученные клинические данные сейчас все еще находятся в стадии изучения, но они свидетельствуют о том, что проведение гипертермии в качестве составляющей мультимодальной схемы лечения, особенно в сочетании с иммунотерапией и инновационными процедурами с таргетной доставкой лекарственных препаратов, повышает показатели выживаемости и улучшает качество жизни пациентов.
Сравнительная статистика методов лечения
При сравнении методов лечения рака эндометрия 4 стадии и оценке их эффективности следует учитывать показатели успешности лечения, показатели выживаемости и стоимость терапии.
| Характеристики/Вид терапии | Показатели 2-летней выживаемости | Показатели ответа на лечение | Продолжительность курса лечения | Побочные эффекты |
|---|---|---|---|---|
| Стандартные методы лечения | ~25% на поздних стадиях рака | Менее 10% | Несколько циклов | Тяжелые побочные эффекты (тошнота, утомляемость, выпадение волос, иммуносупрессия, раздражение кожи) |
| Инновационные методы лечения | ~60% на поздних стадиях рака | 45-65% | До 4 сеансов | Незначительные побочные эффекты (дискомфорт в месте проведения лечебной манипуляции) |
Стоимость лечения рака матки 4 стадии
| Метод лечения | Германия | Великобритания | США |
|---|---|---|---|
| Стандартные методы лечения | €80 000 - €150 000 за полный курс | €90 000 - €165 000 за полный курс | €100 000 - €180 000 за полный курс |
| Инновационные методы лечения | €25 000 - €60 000 за полный курс | €70 000 - €120 000 за полный курс | €100 000 - €150 000 за полный курс |
* В таблице указана приблизительная стоимость лечения стандартными и инновационными методиками. Цены могут значительно отличаться в зависимости от клиники и страны, в которых будет проходить лечение, продолжительности пребывания пациента в стационаре, используемого оснащения и технологий, сложности лечебной процедуры и индивидуальных потребностей пациента.
Истории пациенток об успешном лечении
Рак эндометрия 4 стадии – это серьезный диагноз, но благодаря достижениям в области таргетной терапии, иммунотерапии и альтернативных методов лечения сейчас есть возможность значительно улучшить показатели выживаемости и качество жизни многих пациенток. Реальный опыт пациенток демонстрирует, что интенсивный курс персонализированного лечения способен обеспечить длительную ремиссию и существенно замедлить прогрессирование опухоли, а в некоторых случаях возможно даже полное излечение.
Пациентки, прошедшие процедуры HIPEC и TACE, терапию дендритными клетками или иммунотерапию, подтверждают положительные результаты лечения этими методами: несмотря на позднюю стадию заболевания, некоторым из них удалось достичь длительной ремиссии. Комбинированные схемы лечения, особенно сочетающие стандартную химиотерапию с иммунотерапией или локальными лечебными процедурами, потенциально повышают продолжительности жизни, минимизируя при этом тяжелые побочные эффекты традиционных терапевтических методик.
В Германии принимают на лечение пациенток с клиническим случаями различной тяжести, обеспечивая им современную терапию с хорошим результатом.
Сюзанна Линн О'Донохью на собственном опыте убедилась в исключительно высоком качестве медицинского обслуживания в этой стране. У пациентки диагностировали рак яичников и молочной железы. Благодаря профессиональной помощи специалистов Booking Health ее лечение во Франкфурте прошло максимально гладко и комфортно, весь процесс был хорошо спланирован и скоординирован. Аналогичный позитивный опыт лечения в Германии был и у Гретты Гаспарян, которой диагностировали рак яичников 4 стадии. Пациентка успешно прошла курс иммунотерапии дендритными клетками. Обо всех организационных вопросах и координации лечения позаботились сотрудники Booking Health.
Опыт этих двух женщин и многих других пациенток свидетельствует о важности индивидуального подхода к лечению рака и профессиональной поддержки при поездке на лечение за границу, а также отчетливо демонстрирует огромную роль интегрирования в комплексную схему лечения инновационных методик при борьбе с онкопатологией на последних стадиях.
Поездка на лечение за границу с Booking Health
Самостоятельный поиск наилучшей тактики лечения с учетом вашей индивидуальной клинической ситуации – довольно сложная задача. Испытав на себе многочисленные курсы лечения, проконсультировавшись со множеством специалистов и испробовав различные терапевтические процедуры, вам может быть трудно сориентироваться во всей предоставленной врачами информации. В таком случае пациенты зачастую выбирают первый же предложенный вариант лечения или соглашаются на лечение с применением стандартизированных терапевтических протоколов, которое повлечет за собой множество побочных эффектов, вместо того, чтобы рассмотреть возможность терапии с помощью инновационных процедур.
Если вы хотите сделать осознанный выбор и получить лечение рака в соответствии с индивидуально разработанной для вас схемой с учетом особенностей вашей конкретной клинической ситуации, проконсультируйтесь с врачами-консультантами Booking Health. Компания Booking Health уже более 12 лет занимает ведущие позиции в сфере организации лечения за рубежом с применением новейших инноваций в медицине, поэтому ее специалисты обладают огромным опытом в составлении персонализированных комплексных программ лечения для каждого пациента. Booking Health пользуется репутацией авторитетной компании, которая предоставляет персонализированный подбор схемы лечения рака матки 4 стадии и клиники с прямым бронированием приема в медицинском центре и полной поддержкой на каждом этапе лечения – от решения организационных вопросов до помощи в процессе лечения. Мы предлагаем:
- Оценку и анализ выписок пациентки
- Составление индивидуальной программы лечения
- Подбор подходящего медицинского учреждения для лечения
- Подготовку медицинской документации и ее направление в выбранную пациенткой для лечения клинику
- Консультации с врачами зарубежной клиники для разработки оптимальной медицинской программы на этапе подготовки к поездке на лечение
- Экспертные консультации во время пребывания в больнице
- Последующее консультирование пациентки после ее возвращения на родину по завершении медицинской программы
- Решение организационных вопросов в рамках подготовки к поездке на лечение за границу
- Координацию пребывания пациентки в другой стране, помощь в бронировании отеля или апартаментов на период лечения
- Помощь в оформлении визы и бронировании авиабилетов
- Услуги переводчика и персонального координатора, который будет с вами на связи 24/7
- Прозрачные цены на лечение без скрытых платежей
Здоровье – главная ценность в жизни каждого человека, доверять заботу о которой стоит лишь лучшим специалистам с богатым опытом и проверенной репутацией. Booking Health – это ваш надежный партнер, который оказывает всестороннюю помощь на пути к восстановлению здоровья и улучшению качества жизни. Свяжитесь с врачом-консультантом компании, чтобы узнать больше о возможностях персонализированного лечения метастатического рака матки у ведущих экспертов с использованием инновационных методов.
Современная онкология: опыт пациентов Booking Health
Частые вопросы наших пациенток о раке эндометрия 4 стадии
Отправить запрос на лечениеРак матки 4 стадии – это наиболее тяжелая стадия карциномы эндометрия, при которой рак распространяется за пределы матки на отдаленные органы: легкие, печень, кости или лимфатические узлы. На этой стадии рака происходит распространение метастазов, поэтому для подавления онкопроцесса необходимо проведение системных методов лечения в комбинации с таргетной терапией.
При раке матки 4 стадии пациентки испытывают такие симптомы: боли в области таза, аномальные маточные кровотечения, потерю веса, повышенную утомляемость, затрудненное мочеиспускание, отеки нижних конечностей. При распространении рака на легкие или печень также может появится одышка или желтуха.
При лечении применяются такие стандартные методы, как химиотерапия, лучевая терапия, гормональная терапия, а также такие инновационные методы, как иммунотерапия, терапия дендритными клетками, HIPEC, гипертермия и химиоэмболизация (TACE). Для облегчения симптомов проводится паллиативная терапия.
Прогноз при раке эндометрия 4 стадии зависит от степени распространения опухоли, общего состояния женщины и ответа на лечение. Пятилетняя выживаемость составляет примерно 15-20%, но лечение новаторскими видами таргетной терапии способствует улучшению результатов.
Продолжительность жизни варьируется в зависимости от степени распространения метастазов и эффективности проведенного лечения. При лечении по стандартному протоколу продолжительность жизни составляет 1-3 года, а при использовании инновационных терапевтических методик существует высокая вероятность более существенного повышения показателей выживаемости.
Достижение полной ремиссии маловероятно, но при лечении с помощью таких современных методов, как иммунотерапия, химиоэмболизация и HIPEC, часто удается добиться длительной ремиссии или стабилизации заболевания.
В отличие от более ранних стадий заболевания, при раке матки 4 стадии происходит распространение онкопроцесса на отдаленные органы, на фоне чего снижается эффективность локализованных методов лечения, например, хирургического вмешательства. В таком случае на первый план выходит лечение при помощи системных методов.
Чаще всего при раке матки 4 стадии онкопроцесс распространяется на легкие, печень, кости, лимфатические узлы и брюшину.
Выбирайте лечение за рубежом и Вы, несомненно, получите отличный результат!
Авторы:
Статья составлена под редакцией экспертов в области медицины, врачей-специалистов доктора Надежды Иванисовой и доктора Богдана Михальнюка. Для лечения состояний, о которых идет речь в статье, необходимо обратиться к врачу; информация в статье не предназначена для самолечения!
С редакционной политикой, которая отражает наше стремление к точности и прозрачности, можно ознакомиться здесь. Перейдите по ссылке, чтобы ознакомиться с нашими правилами.
Источники:
National Institutes of Health (NIH)
Читайте:
Комплексное руководство по методам лечения рака яичников
Комплексное руководство по лечению рака молочной железы 4 стадии: возможности терапии
Меню статьи:
Не знаете, с чего начать?
Свяжитесь с Booking Health